唐朝晖
[摘要] 目的 探讨孕期内TPO-Ab阴性的亚甲减对初产妇妊娠和分娩结局的影响。 方法 选取2017年8月~2018年8月于我院明确诊断为亚临床甲减的207例初产妇作为实验对象,根据孕期分为A、B、C三组,采用化学发光免疫分析法测定血清中TSH水平,记录并比较三组实验对象TSH水平,并随访三组实验对象的妊娠和分娩结局。结果 三组实验对象血清中的TSH水平存在明显差异(P<0.05);随访三组的妊娠结局发现,A、B、C三组妊娠期糖尿病、胎膜早破、妊娠期贫血、产后出血及早产的发生率比较,差异有统计学意义(P<0.05),另外A、B、C三组妊娠期间发生妊娠期高血压、前置胎盘等方面的概率无明显差异(P>0.05);观察三组实验对象胎儿情况发现,A、B、C三组的胎儿发生低出生体重及新生儿生长受限的概率,差异有统计学意义(P<0.05),而A、B、C三组胎儿发生巨大儿、胎内呼吸窘迫等方面的概率无明显差异(P>0.05)。 结论 TPO-Ab阴性的亚临床甲减的初产妇在不同孕期产生TSH的定量不同,从而影响产妇的妊娠结局及胎儿的情况,因此对不同孕期TSH的监测及控制对TPO-Ab阴性的亚临床甲减初产妇的妊娠及分娩结局具有重要的意义,值得在临床上极力推广。
[关键词] 不同孕期;亚甲减;初产妇;妊娠和分娩结局
[中图分类号] R714.2 [文献标识码] B [文章编号] 1673-9701(2020)12-0064-04
[Abstract] Objective To explore the effect of TPO-Ab-negative subclinical hypothyroidism during pregnancy on pregnancy and delivery outcomes in primiparas. Methods A total of 207 primiparas who were clearly diagnosed with subclinical hypothyroidism in our hospital from August 2017 to August 2018 were selected as experimental subjects. They were divided into three groups of A, B, and C according to pregnancy terms. Chemiluminescence immunoassay was used to determine the level of TSH in serum. The TSH levels were recorded and compared between the three groups of subjects, and the pregnancy and delivery outcomes of the three groups of subjects were followed up. Results The TSH levels of the three groups of subjects were compared, and it was found that there were significant differences in the serum TSH levels between the three groups of subjects, and the differences were statistically significant(P<0.05); During the follow-up of the pregnancy outcomes of the three groups, the incidence rates of gestational diabetes, premature rupture of membranes, anemia during pregnancy, postpartum hemorrhage and preterm birth were different between group A, group B and group C, and the differences were statistically significant(P<0.05). In addition, there was no significant difference in the incidence rate of pregnancy-related hypertension and placenta previa during pregnancy in the three groups of A, B, and C, and the differences were not statistically significant(P>0.05); The infants in the three groups of subjects were observed, and it was found that the incidence rates of low birth weight infant and neonatal growth restriction were different in group A, B and C, and the differences were statistically significant(P<0.05). However,there was no significant difference in the probability of fetal giantness and intra-natal respiratory distress among the three groups of A, B, and C, and the differences were not statistically significant(P>0.05). Conclusion The quantity of TSH produced by primiparas with TPO-Ab-negative subclinical hypothyroidism is different in different pregnancy trimesters, which affects the pregnancy outcome of the puerpera and the condition of the infants. Therefore, the monitoring and control of TSH in different pregnancy trimemsters is of great significance to the pregnancy and delivery outcomes of primiparas with TPO-Ab-negative subclinical hypothyroidism, and it is worthy of clinical promotion.
[Key words] Pregnancy trimesters; Subclinical hypothyroidism; Primiparas; Pregnancy and delivery outcomes
亚临床甲状腺功能减退(Subclinical hypothyroidi-sm,SCH)是一定原因引起的机体内甲状腺激素降低,从而引起TSH升高,但是总甲状腺激素处于正常范围内的一类疾病,一般无明显症状[1]。甲状腺激素是人体内促进生长发育的重要激素,妊娠期由于对甲状腺激素需求量较大,容易引起亚临床甲状腺功能减退,因此妊娠期合并亚临床甲减的发病率较高[2-3]。大量研究表明,妊娠期合并亚临床甲减可导致孕妇发生妊娠期糖尿病、早产等结局,同时对胎儿的生长发育有一定的影响,主要致病因素和甲状腺激素减少以及TPO-Ab的侵袭关系较大。但是妊娠期不同时期体内对甲状腺激素的需求不一,发生亚临床甲减的程度也各不相同,因此探究不同孕期发生亚甲减对孕妇的妊娠和分娩结局具有重要的意义[4],但临床上此类研究较少,故设计此次实验。本实验通过排除TPO-Ab的影响探讨不同孕期发生亚甲减对初产妇妊娠结局及胎儿情况的影响,现报道如下。
1 资料与方法
1.1 一般资料
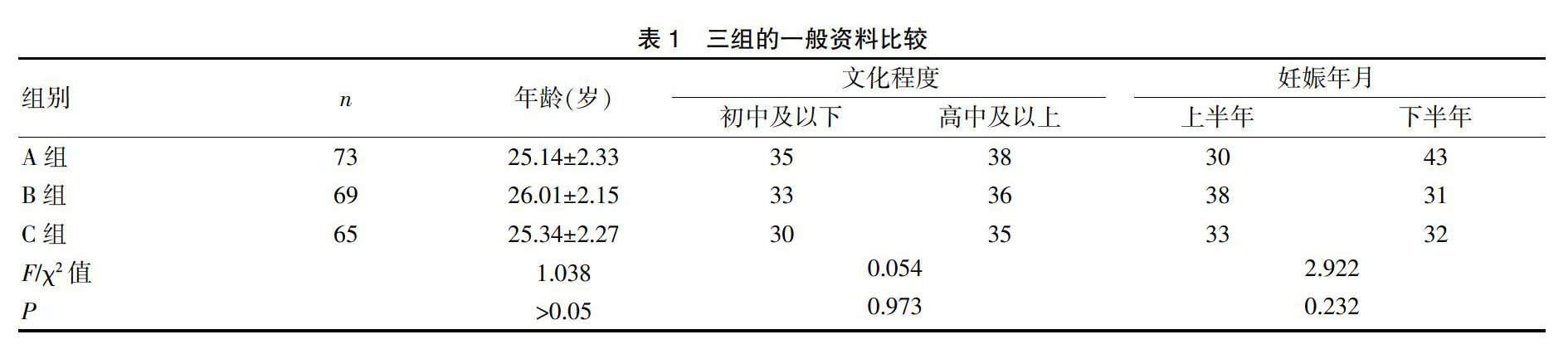
选取2017年8月~2018年8月于我院明确诊断为亚临床甲减的207例孕妇作为实验对象,根据不同孕周分为A、B、C三组,其中73例在妊娠4~12周时发现亚临床甲减的孕妇作为A组,69例在妊娠13~28周时发现亚临床甲减的孕妇作为B组,65例在妊娠29~40周发现亚临床甲减的孕妇作为C组。纳入标准:(1)所有实验对象均为初产妇;(2)所有实验对象外周血内TPO-Ab均为阴性;(3)孕周均按照末次月经计算,同时予以超声纠正孕周;(4)年龄分布在20~35岁;(5)均为单胎妊娠;(6)向患者交代具体目的及相关风险后签署知情同意书并通过医院伦理委员会审查;排除标准:(1)患有糖尿病、高血压等基础疾病;(2)多胎妊娠;(3)有家族性遗传病;(4)地方性甲状腺肿区域生活史;(5)拒绝随访[5]。A、B、C三组间实验对象的年龄、文化程度及妊娠时间比较,差异无统计学意义(P>0.05),具有可比性。见表1。
1.2 诊断标准
采用美国甲状腺协会(American thyroid association,ATA)标准进行诊断,TSH正常参考值范围孕早期为0.1~2.5 mIU/L,孕中期为0.2~3.0 mIU/L,孕晚期为0.3~3.0 mIU/L,因此孕早期TSH>2.5 mIU/L、孕中晚期TSH>3.0 mIU/L即可诊断妊娠期亚临床甲状腺功能减退[6]。
1.3 方法
所有实验对象夜间10点后禁食水,于凌晨6点采用同一批号的采血器抽取静脉血10 mL,采集完毕后将标本送至实验室,采用化学发光免疫分析法测定血清中TSH水平,使用全自动化学发光法免疫分析仪(型号:CHEMCLIN1500,北京科美生物技术有限公司)及TSH测定试剂盒(北京科美生物技术有限公司)测定所有实验对象的TSH水平[7-8]。
1.4 观察指标
(1)记录并比较三组实验对象血清中TSH水平;(2)随访三组实验对象的妊娠结局,比较在不同孕期发生妊娠期糖尿病、妊娠期高血压、前置胎盘、胎盘早剥、胎膜早破、妊娠期贫血、胎位异常、羊水异常、脐带异常、肝内胆汁淤积、宫缩异常、产后出血、早产的情况;(3)随访三组实验对象胎儿情况,比较三组间胎儿发生低出生体重儿、巨大儿、胎儿宫内呼吸窘迫、胎儿畸形、新生儿窒息、新生儿生长受限、新生儿先天性甲减、胎死宫内的情况[9-10]。
1.5 统计学方法
采用SPSS 18.0统计软件对实验数据进行分析处理,计量资料用(x±s)表示,多组间计量资料比较进行方差分析,计数资料以[n(%)]表示,组间采用χ2检验,P<0.05为差异有统计学意义。
2 结果
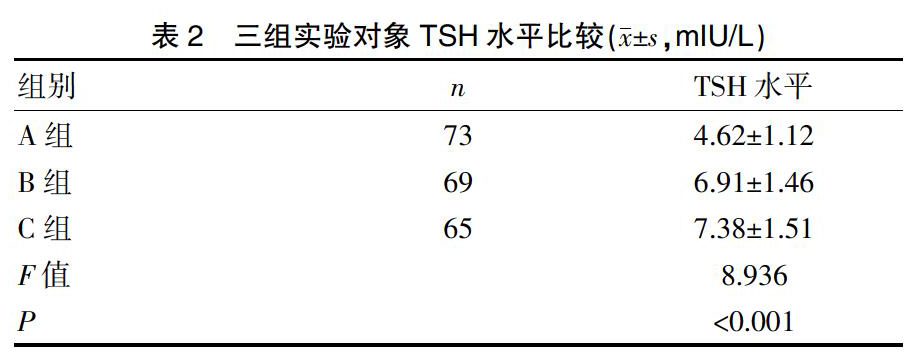
2.1 三组实验对象TSH水平比较
三组实验对象血清中的TSH水平存在明显差异(P<0.05)。见表2。
2.2 三组实验对象妊娠结局比较
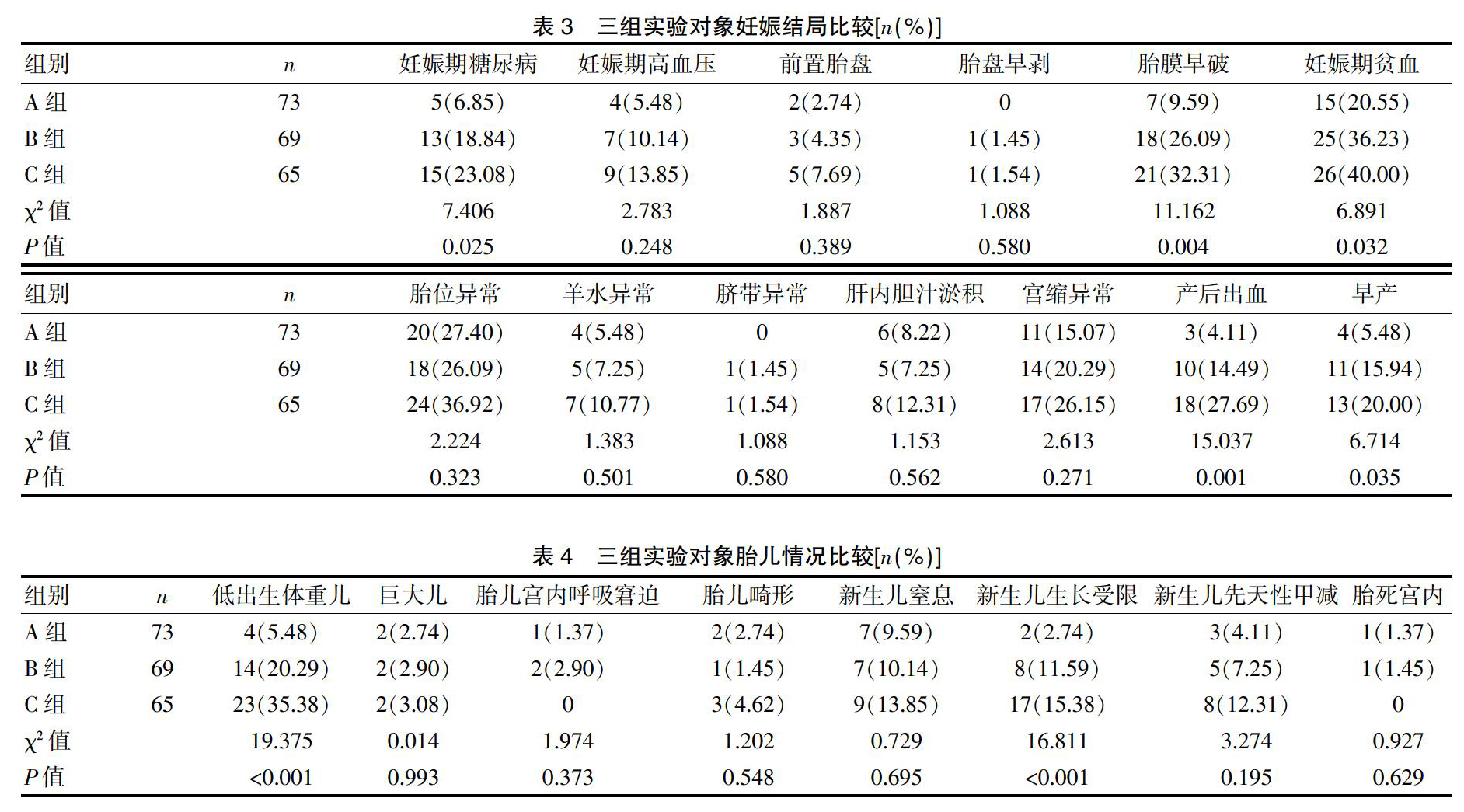
通过随访三组实验对象的妊娠结局发现,B、C两组妊娠期糖尿病、胎膜早破、妊娠期贫血、产后出血及早产的发生率比A组高,差异有统计学意义(P<0.05),而B、C两组妊娠期糖尿病、胎膜早破、妊娠期贫血、产后出血及早产的发生率无明显差异,差异无统计学意义(P>0.05),另外A、B、C三组妊娠期间发生妊娠期高血压、前置胎盘、胎盘早剥、胎位异常、羊水异常、脐带异常、肝内胆汁淤积、宫缩异常的概率比较,差异无统计学意义(P>0.05)。见表3。
2.3 三组实验对象胎儿情况比较
通过观察三组实验对象胎儿情况发现,B组和C组实验对象的胎儿发生低出生体重及新生儿生长受限的概率大于孕早期A组,差异有统计学意义(P<0.05),同时C组实验对象的胎儿发生低出生体重及新生儿生长受限的概率大于B组的实验对象,差异有统计学意义(P<0.05),而A、B、C三组胎儿发生巨大儿、胎内呼吸窘迫、胎儿畸形、新生儿窒息、新生儿先天性甲减、胎死宫内的概率比较,差异无统计学意义(P>0.05)。见表4。
3 讨论
甲状腺激素是促进骨骼和神经系统的重要激素,甲状腺激素减少时,机体会通过下丘脑-垂体-甲状腺轴调节机体内的甲状腺激素,从而维持在正常水平[11]。妊娠合并亚临床甲状腺功能减退是甲状腺功能减退的早期阶段,发病率为2%~3%,其临床表现不显著,因此极易被漏诊或误诊[12]。妊娠合并亚甲减的孕妇体内甲状腺激素降低,通过负反馈调节机体产生大量的TSH,促进甲状腺激素的生成,因此总甲状腺激素维持在正常水平[13-14]。不同孕期发生亚临床甲减时机体缺乏甲状腺激素的程度不同,为维持总甲状腺激素的稳定,机体产生TSH的数量也不相同,根据ATA诊断标准,孕早期TSH>2.5 mIU/L、孕中晚期TSH>3.0 mIU/L即可诊断妊娠期亚临床甲状腺功能减退。大量研究数据表明,妊娠合并亚甲减会导致不同的妊娠结局及对胎儿会产生一定的影响,其原因目前尚未明确,其中TPO-Ab、甲状腺激素和TSH水平的高低、不同孕周均有可能,有实验数据表明,TPO-Ab阳性的亚甲减合并妊娠对妊娠结局和胎儿存在一定的影响,但不同孕期发生亚甲减的妊娠结局和胎儿情况缺乏临床数据[15-16]。本实验通过排除TPO-Ab的影响探究不同孕期发生亚甲减对初产妇妊娠结局及胎儿情况的影响。
本实验结果显示,三组实验对象的TSH水平比较,三组实验对象血清中的TSH水平存在明显差异(P<0.05),不同孕期对甲状腺激素的需求不同,导致妊娠合并亚甲减的初产妇体内TSH水平不同,随着孕周的增加,甲状腺激素需求增加,因此TSH水平越高,但孕中期及孕晚期之间无明显差异;随访三组实验对象的妊娠结局发现,B、C两组妊娠期糖尿病、胎膜早破、妊娠期贫血、产后出血及早产的发生率比A组高,差异有统计学意义(P<0.05),而B、C两组妊娠期糖尿病、胎膜早破、妊娠期贫血、产后出血及早产的发生率无明显差异,差异无统计学意义(P>0.05),其发生机制尚不能明确,妊娠期糖尿病的发生可能与甲状腺激素的降低增加了胰岛素的抵抗,而胎膜早破、妊娠期贫血、产后出血及早产可能是由于TSH以及甲状腺激素对下丘脑产生作用,从而影响其他激素的相关调节;另外A、B、C三组妊娠期间发生妊娠期高血压、前置胎盘、胎盘早剥、胎位异常、羊水异常、脐带异常、肝内胆汁淤积、宫缩异常的概率无明显差异(P>0.05);观察三组实验对象胎儿情况发现,B组和C组实验对象的胎儿发生低出生体重及新生儿生长受限的概率大于孕早期A组,差异有统计学意义(P<0.05),同时C组实验对象的胎儿发生低出生体重及新生儿生长受限的概率大于B组的实验对象,差异有统计学意义(P<0.05),这是由于甲状腺激素是促进生长发育的重要激素,因此妊娠合并亚甲减的初产妇分娩的胎儿在生长发育方面受到一定的影响;而A、B、C三组胎儿发生巨大儿、胎内呼吸窘迫、胎儿畸形、新生儿窒息、新生儿先天性甲减、胎死功能的概率无明显差异(P>0.05)[17-19]。因此在不同孕期调整TPO-Ab阴性的亚甲减初产妇体内的甲状腺激素及TSH,对妊娠结局及胎儿的影响具有重要意义。
本研究不足之处,首先本研究的样本量较少,其代表性具有一定的局限性;其次本实验为探究甲状腺激素及TSH对下丘脑其他激素的影响,力争在接下来的实验中探究相互关系佐证本次研究结果;最后仍需要更多的临床数据来评估不同孕期内外周血内TPO-Ab阴性的亚甲减对初产妇妊娠和分娩结局影响[20]。
[参考文献]
[1] 刘晓红,高素红,王佳楣,等.亚临床甲状腺异常对妊娠结局的影响[J].中华围产医学杂志,2012,15(11):696-700.
[2] Sharmeen M,Shamsunnahar PA,Laita TR,et al. Overt and subclinical hypothyroidism among Bangladeshi pregnant women and its effect on fetomaternal outcome[J].Bangladesh Medical Research Council Bulletin,2014,40(2):52.
[3] Sally M Reid, Philippa Middleton,Mary C Cossich,et al. Interventions for clinical and subclinical hypothyroidism pre-pregnancy and during pregnancy[J]. Cochrane Database of Systematic Reviews,2013,5(5):CD007752.
[4] 中华医学会内分泌学分会,中华医学会围产医学分会.妊娠和产后甲状腺疾病诊治指南[J].中华内分泌代谢杂志,2012,28(5):354-371.
[5] Bannerman,Gyamfi C.Basic science and clinical evidence regarding treatment of subclinical hypothyroidism during pregnancy[J].Clinical Obstetrics and Gynecology,2011,54(3):488-492.
[6] Fadeyev VV. Guidelines of the American thyroid association for the diagnosisand management of thyroid disease during pregnancy and postpartum[J]. Thyroid,2012,8(1):1081-1125.
[7] 贺译平,贺同强,王艳霞,等.不同标准诊断的亚临床甲状腺功能减退症及甲状腺过氧化物酶抗体阳性对妊娠的影响[J].中华妇产科杂志,2014,49(11):823-828.
[8] Ma L,Qi H,Chai X,et al. The effects of screening and intervention of subclinical hypothyroidism on pregnancy outcomes:A prospective multicenter single-blind, randomized,controlled study of thyroid function screening test during pregnancy[J]. The Journal of Maternal-Fetal & Neonatal Medicine,2015,29(9):1391-1394.
[9] Wang S,Teng WP,Li JX,et al. Effects of maternal subclinical hypothyroidism on obstetrical outcomes during early pregnancy[J]. Journal of Endocrinological Investigation,2012,35(3):322-325.
[10] 李建新,王森,单忠艳,等.妊娠早期母体甲状腺功能及其抗体异常对妊娠结局的影响[J].中华内分泌代谢杂志,2012,27(11):916-919.
[11] 何玉花,吴敏,徐凤英.妊娠早期抗甲状腺过氧化物酶阴性亚临床甲状腺功能减退症妊娠结局研究[J].中国实用妇科与产科杂志,2019,35(3):87-90.
[12] Cruz-Cruz EA,Aurora Ramírez-Torres,Pimentel-Nieto D,et al.Prevalence of clinical and subclinical hypothyroidism during pregnancy in a pregnant women population[J]. Ginecologíay Obstetricia De México,2014,82(11):717-724.
[13] Stagnaro-Green A.Second trimester levothyroxine treatment for subclinical hypothyroidism or hypothyroxinaemia of pregnancy does not improve cognitive outcomes of children[J]. Evidence Based Medicine,2017,22(4):149-152.
[14] Jayaraman M,Verma A,Harikumar KVS,et al. Pregnancy outcomes with thyroxine replacement for subclinical hypothyroidism:Role of thyroid autoimmunity[J]. Indian J Endocrinal Metab,2013,17(2):294-297.
[15] 徐冬岩,蒋鸿阳,张宏宇,等.甲状腺过氧化物酶抗体阴性的妊娠期亚临床甲状腺功能减退症对妊娠结局及新生儿的影响[J].中国妇幼保健,2016,(24):5344-5347.
[16] Hamblin PS,Sheehan PM,Allan C,et al. Subclinical hypothyroidism during pregnancy:The melbourne public hospitals consensus[J].Internal Medicine Journal,2018, 63(12):612-615.
[17] Maraka S,OKeeffe,Derek T,et al.Subclinical hypothyroidism during pregnancy—should you expect this when you are expecting?[J].JAMA Internal Medicine,2015,175(7):1088.
[18] 佘广彤,王慧艳,陈丽云,等.妊娠晚期亚临床甲状腺功能减退症对妊娠结局的影响[J].中华围产医学杂志,2014,17(11):738-742.
[19] 林森,唐少华,詹爱霞,等.不同孕期和年龄孕妇甲状腺功能指标的比较研究[J].预防医学,2014,(2):137-140.
[20] 卫蔷,张力,刘兴会,等.妊娠不同时期甲状腺功能指标参考值的临床分析[J].中华妇产科杂志,2018,53(5):299-303.
(收稿日期:2019-12-09)



