李肖亮 陈科 莫非 刘传明 杨鹏
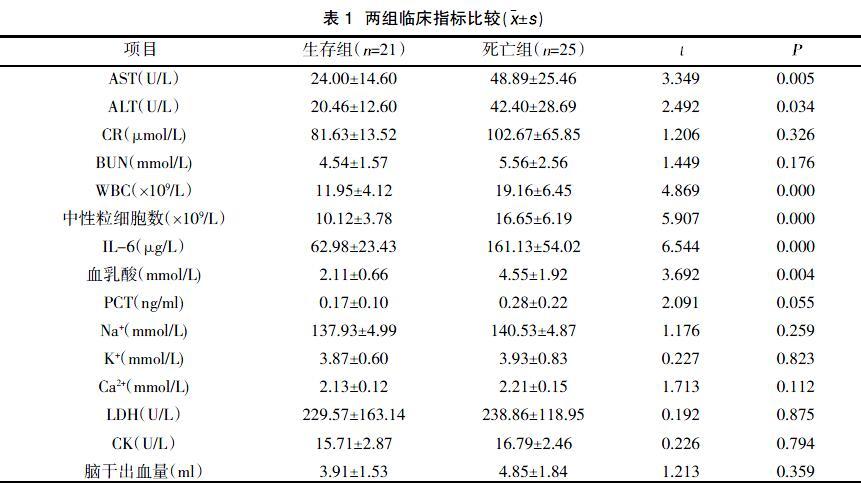
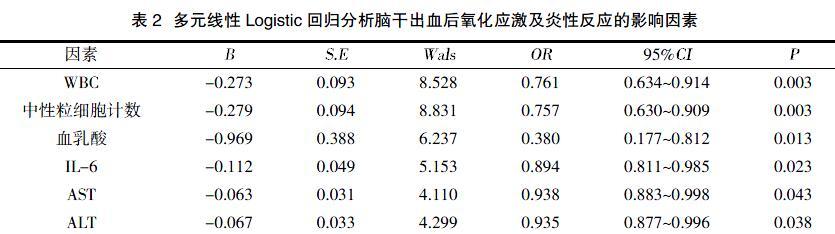
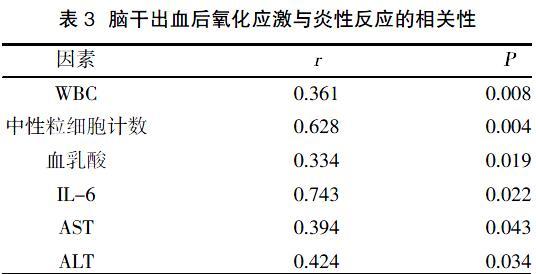
摘要:目的 探讨脑干出血急性期氧化应激和炎性反应的相关性。方法 收集2015年10月~2018年10月我院收治的脑干出血患者46例,依照中国脑出血诊疗指导规范分为死亡组(25例)和生存组(21例)。比较两组天门冬氨酸转氨酶(AST)、丙氨酸氨基转移酶(ALT)、肌酐(CR)、尿素氮(BUN)、白细胞计数(WBC)、降钙素原(PCT)、白介素6(IL-6)、血乳酸、中性粒细胞计数、钠离子(Na)、钾离子(K)、钙离子(Ca)、乳酸脱氢酶(LDH)、肌酸激酶同工酶(CK-MB)、脑干出血量,分析脑干出血后氧化应激及炎性反应的相关性。结果 两组CR、BUN、PCT、Na、K、Ca、LDH、CK-MB、脑干出血量比较,差异无统计学意义(P>0.05);两组AST、ALT、WBC、中性粒细胞计数、IL-6比较,差异有统计学意义(P<0.05)。Spearman相关性分析结果显示,WBC、中性粒细胞计数、血乳酸、IL-6、AST、ALT与脑干出血后氧化应激呈正相关(P<0.05)。多元线性Logistic回归结果显示,WBC、中性粒细胞计数、血乳酸水平、IL-6是脑干出血后氧化应激的独立危险因素。结论 WBC、中性粒细胞计数、血乳酸水平、IL-6是脑干出血后氧化应激的独立危险因素,可用于脑干出血急诊的早期发现和干预,从而提高脑干出血急诊救治成功率,进一步降低死亡率和致残率。
关键词:脑干出血;炎性指标;氧化应激;急诊救治;预后
中图分类号:R743.34 文献标识码:A DOI:10.3969/j.issn.1006-1959.2019.20.017
文章编号:1006-1959(2019)20-0060-04
Correlation between Oxidative Stress and Inflammatory Response in
Acute Stage of Brain Stem Hemorrhage
LI Xiao-liang,CHEN Ke,MO Fei,LIU Chuan-ming,YANG Peng
Abstract:Objective To investigate the correlation between oxidative stress and inflammatory response in the acute phase of brain stem hemorrhage. Methods 46 patients with brain stem hemorrhage admitted to our hospital from October 2015 to October 2018 were enrolled. According to the guidelines for diagnosis and treatment of cerebral hemorrhage in China, they were divided into death group (25 cases) and survival group (21 cases). Comparison of two groups of aspartate aminotransferase (AST), alanine aminotransferase (ALT), creatinine (CR), urea nitrogen (BUN), white blood cell count (WBC), procalcitonin (PCT), interleukin 6 ( IL-6), blood lactate, neutrophil count, sodium ion (Na), potassium ion (K), calcium ion (Ca), lactate dehydrogenase (LDH), creatine kinase isoenzyme (CK-MB ), the amount of brain stem bleeding, analysis of the correlation between oxidative stress and inflammatory response after brain stem hemorrhage. Results There were no significant differences in CR, BUN, PCT, Na, K, Ca, LDH, CK-MB, and brain stem bleeding between the two groups (P>0.05). AST, ALT, WBC, and neutrophil counts in the two groups. Compared with IL-6, the difference was statistically significant (P<0.05). Spearman correlation analysis showed that WBC, neutrophil count, blood lactate, IL-6, AST, ALT were positively correlated with oxidative stress after brain stem hemorrhage (P<0.05). Multivariate linear logistic regression showed that WBC, neutrophil count, blood lactate level, and IL-6 were independent risk factors for oxidative stress after brain stem hemorrhage.Conclusion WBC, neutrophil count, blood lactate level and IL-6 are independent risk factors for oxidative stress after brain stem hemorrhage. They can be used for early detection and intervention of emergency treatment of brain stem hemorrhage, thus improving the success rate of emergency treatment of brain stem hemorrhage. To further reduce mortality and disability.
脑出血后血肿周围区域存有大量浸润性巨噬细胞,增加心脏和血清中ICAM-1、MCP-1、IL-1的表达,同时增加了脑出血后炎症细胞(白细胞和巨噬细胞)向心脏的浸润,增加心脏组织炎症因子的表达,但脑干出血相关炎性反应报道甚少[12]。Wei L等[13]对脑出血后小鼠的脑-心相互作用研究发现,来自受损心肌的炎症因子与脑组织产生的炎症因子有协同作用,在小鼠没有原发性心脏病的情况下,脑出血增加了心脏组织中心脏氧化应激和炎症因子的表达,诱导小鼠出现明显的进行性心功能障碍,并伴有心脏纤维化、心肌细胞肥大和凋亡的增加,证明脑出血可诱导进行性心脏缺血。Okamoto K等[14]报道1例长期反复脑出血患者脑桥和中脑内可见大量AT8免疫反应神经元和突起,提示氧化应激可能加速脑干磷酸化tau蛋白的积累。
本研究中两组AST、ALT比较,差异有统计学意义(P<0.05),说明神经系统和免疫系统相互影响,但脑干出血患者心肌损伤表现(LDH、CK-MB)未见明显差异,可能与脑干出血早期/超早期氧化应激损伤尚未波及心血管系统有关,相关机制尚待进一步研究。
综上所述,WBC、中性粒细胞计数、血乳酸水平、IL-6是脑干出血后氧化应激的独立危险因素,可用于脑干出血急诊的早期发现和干预,从而提高脑干出血急诊救治成功率,进一步降低死亡率和致残率。
参考文献:
[1]杨树源,张建宁.神经外科学[M].北京:人民卫生出版社,2015.
[2]中华医学会神经病学分会.中国脑出血诊治指南[J].中华神经科杂志,2015,48(6):435-444.
[3]Murakami M,Fujioka S,Oyama T,et al.Serial changes in the regional cerebral blood flow of patients with hypertensive intracerebral hemorrhage:long-term follow-up SPECT study[J].J Neurosurg Sci,2015,49(3):117-124.
[4]Ordónez-Rubiano EG,Johnson JM,Younus I,et al.Recovery of consciousness after a brainstem cavernous malformation hemorrhage:A descriptive study of preserved reticular activating system with tractography[J].Journal of Clinical Neuroscience,2019(59):372-377.
[5]Lekic T,Rolland W,Manaenko A,et al.Evaluation of the hematoma consequences,neurobehavioral profiles,and histopathology in a rat model of pontine hemorrhage[J].J Neurosurg,2013,118(2):465-477.
[6]李敬,李颖,郭丽娟,等.脑干出血并发脑心综合征心律失常与儿茶酚胺浓度的临床分析[J].中国现代医学杂志,2016,26(23):59-62.
[7]Schneider U,Davids A,Brandenburg S,et al.Microglia inflict delayed brain injury after subarachnoid hemorrhage[J].Acta Neuropathol,2015,130(2):215-231.
[8]Wakai T,Sakata H,Narasimhan P,et al.Transplantation of neural stem cells that overexpress SOD1 enhances amelioration of intracerebral hemorrhage in mice[J].J Cereb Blood Flow Metab,2014,34(3):203-215.
[9]Mewhort HE,Lipon BD,Svystonyuk DA,et al.Monocytes increase human cardiac myofibroblast-mediated extracellular matrix remodeling through TGF-beta1[J].Am J Physiol Heart Circ Physiol,2016(310):716-724.
[10]Zhou F,Jiang Z,Yang B,et al.Magnolol exhibits anti-inflammatory and neuroprotective effects in a rat model of intracerebral haemorrhage[J].Brain Behav Immun,2018(12):28.
[11]Erdi F,Keskin F,Esen H,et al.Telmisartan ameliorates oxidative stress and subarachnoid haemorrhage-induced cerebral vasospasm[J].Neurol Res,2016,38(3)626-641.
[12]Lin L,Yihao T,Zhou F,et al.Inflammatory regulation by driving microglial M2 polarization:neuroprotective effects of cannabinoid receptor-2 activation in intracerebral hemorrhage[J].Front Immunol,2017(8):112-119.
[13]Wei L,Lilin L,Michael C,et al.Intracerebral Hemorrhage Induces Cardiac Dysfunction in Mice Without Primary Cardiac Disease[J].Front Neurol,2018(9):965-973.
[14]Okamoto K,Naito I,Fukuda T,et al.Adult moyamoya disease associated with abundant phosphorylated tau accumulation in the brainstem:Report of a case with autopsy findings[J].Neuropathology,2018,38(3):224.
收稿日期:2019-5-6;修回日期:2019-6-10
编辑/杜帆



