曾振华 严敏 戴仪 邓硕 邹三宝 尹君
·临床研究·
CT引导下靶点射频联合臭氧注射消融术治疗颈椎间盘突出症临床研究
曾振华 严敏 戴仪 邓硕 邹三宝 尹君
目的 探讨CT引导下靶点射频联合臭氧注射消融术治疗颈椎间盘突出症的临床疗效及安全性。方法 回顾性分析542例应用靶点射频热凝联合臭氧注射进行颈椎间盘突出症治疗患者的临床资料。采用视觉模拟疼痛评分(VAS)评价患者的疼痛程度并进行治疗效果评估。结果 术后24h、1周、1、3、6个月的优良率分别为85.9%、79.9%、85.4%、86.9%、86.3%。与术前比较,术后各时间点的VAS评分明显降低(P<0.05)。患者术中、术后无一例发生严重并发症。结论 CT引导下靶点射频联合臭氧注射消融术创伤小、安全性高,是治疗颈椎间盘突出症的有效方法。
靶点射频热凝术 臭氧注射消融术 颈椎间盘突出
颈椎间盘突出症是临床上较为常见的脊柱疾病,可导致患者出现颈肩背部疼痛、麻木及头晕头痛等一系列临床症状,严重影响患者的工作及生活[1]。目前,针对颈椎间盘突出症治疗的方法较多,如骨科手术治疗、低温等离子射频消融术等[2-3]。而射频热凝术在脊柱微创介入手术中应用广泛且方法多样[4-5],其在颈椎间盘的微创介入治疗中是最常用的手段[6];臭氧注射治疗颈椎间盘突出症也有确切的疗效[7-8]。研究报道,靶点射频联合臭氧注射消融术治疗颈椎间盘突出症,具有疗效好、安全性高、费用相对低廉等特点[9]。作者采用靶点射频热凝联合臭氧消融术治疗颈椎间盘突出症,取得良好的疗效,现报道如下。
1 临床资料
1.1 一般资料 2005年10月至2015年9月颈椎间盘突出症患者542例,其中男375例,女167例;年龄37~76岁,病程6个月至12年,经保守治疗无效。384例有上肢麻木史(其中单侧上肢麻木327例;双侧上肢麻木57例);158例伴有单侧或双侧上肢肌力Ⅲ~Ⅳ级;霍夫曼征阳性32例;302例伴有腱反射减弱;C3~4椎间盘突出164例,C4~5椎间盘突出351例,C5~6椎间盘突出387例,C6~7椎间盘突出326例,2个椎间盘同时突出255例,3个椎间盘同时突出282例,共介入治疗椎间盘1079个。纳入与排除标准:(1)入选标准:术前颈椎MRI或CT显示为C3~4、C4~5、C5~6或C6~7椎间盘突出,突出类型为旁中央突出、侧后方突出或椎间盘膨出,临床表现为一侧或双侧颈肩部、上肢疼痛和(或)麻木。影像学检查和临床表现相符。(2)排除标准:脊髓型、交感型和椎动脉型颈椎病,受压节段颈髓内缺血、软化,颈椎管骨性狭窄、严重颈椎骨质增生,椎间盘突出钙化,伴严重心肺疾病,凝血功能异常,臭氧使用禁忌等。
1.2 方法 根据术前颈椎X线平片,找出目标椎间盘,计算好该靶点的相应位置,明确穿刺途径及深度。患者入手术室后取后仰位,常规生命体征监测,建立液体通路,并静脉滴注抗生素和止吐药。CT引导下,采用前路20G射频针经颈前血管鞘和气管鞘之间穿刺入目标椎间盘,经CT确认穿刺针已达靶点,拔出针芯,回抽无脑脊液、血液,间盘内注入50μl/ml的臭氧2~5ml。然后用射频仪(医科达AB)分别给予高频电流(50HZ,0.8~1.0mA)进行感觉测试和低频电流(2HZ,0.8~2.0mA)进行运动测试。经测试未引出支配区疼痛和运动后,依次给予60℃,70℃,80℃,90℃从低到高的射频热凝各15s以测定患者能够耐受的最高温度。采用患者能够耐受的最高温度治疗4周期(60s/周期)。患者治疗后需绝对卧床24h,24h后可在颈托辅助下下地活动。常规给予神经营养及脱水治疗3d。
1.3 疗效标准 (1)根据VAS评分法评定患者治疗前后各时期(术后24h、1周、1、3、6个月)疼痛程度的变化。(2)依据改良MacNab腰腿痛手术评价标准进行评价[10]:优:疼痛消失,能参加工作和运动,恢复正常工作;良:偶有腰背痛或坐骨神经痛,不影响工作;中:症状缓解不彻底,需要药物治疗;差:症状无改进,体力活动受限。(3)优良率为优和良之和;失败率为差和无效之和。
1.4 统计学分析 采用SPSS17.0 统计软件。计量资料采用(x±s)表示,组内比较采用重复测量数据的方差分析。以P<0.05为差异有统计学意义。
2 结果
2.1 治疗前后VAS评分比较 与治疗前VAS评分比较,治疗结束后24h、1周、1、3、6个月VAS评分均显着下降(P<0.05)。见表1。
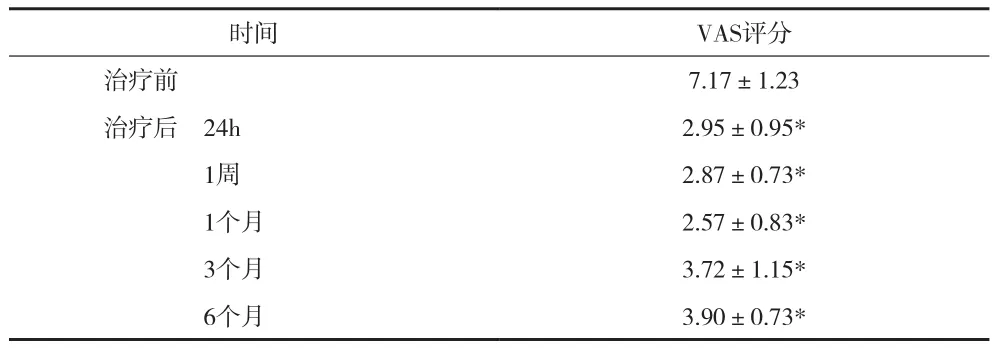
表1 治疗前后VAS评分比较(x±s)
2.2 患者治疗后不同时间点临床效果 见表2。
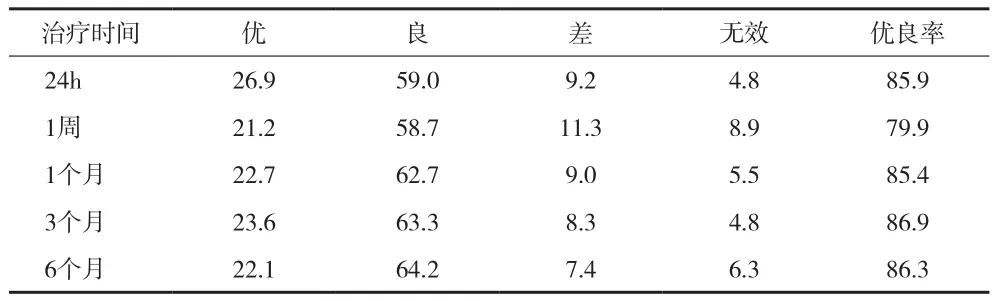
表2 患者治疗后不同时间点临床效果(%)
3 讨论
椎间盘突出症可见于脊柱的任何节段,但多见于颈椎及腰椎[11-12]。颈椎间盘突出症是在颈椎间盘退变的基础上,因累加轻微外力或无明确诱因导致椎间盘突出而致脊髓和神经根受压产生相应症状的临床症候群,是临床引起颈肩痛常见原因之一[13]。研究显示,颈椎间盘突出症的间盘退变程度一般较颈椎病的骨性退变轻,在颈椎间盘退变的早期进行干预,不仅可以缓解及治疗由其引起的临床症状,且可阻止或延缓因椎间盘退变而继发的一系列病变[14]。因此,颈椎间盘突出症的早期治疗不仅有助于去除疾病本身的病变,也有助于预防相关并发症的发生。
MRI是诊断颈椎间盘突出症的首选方法。然而,MRI对于椎体前缘的软性椎间盘突出物与骨赘分辨存在困难,在椎间孔附近表现更为明显,在一定程度上降低MRI的诊断效能[15]。CT检查因其可提供清晰的横断面影像,对椎管内软性椎间盘突出物与骨赘、黄韧带等结构有较高的分辨率,在诊断颈椎间盘突出症有特殊的价值。因此,通过CT引导下进行的穿刺治疗,使穿刺针直接达到目标靶点,大幅提高穿刺的准确性和安全性,有利于对软性突出物的精准治疗。
椎间盘突出症的治疗手段众多,传统的保守疗法不能去除突出的椎间盘,只能缓解症状,存在易复发的缺点。外科手术能够去除病因,然而创伤大、并发症多及远期效果不理想的缺点,限制其临床应用。近年来,颈椎间盘突出症的介入治疗发展迅速,受到越来越多患者及医师的重视。
射频热凝靶点消融术是将射频电流直接作用于突出的颈椎间盘,使局部温度升高,导致部分髓核组织变性、凝固萎缩,从而降低椎间盘内压力,达到对椎间盘周围组织神经根、动脉、脊髓等的减压目的。此外,热凝效应还有助于减轻炎性反应,减少针道感染,灭活致痛因子,可进一步减轻患者的症状[16]。值得注意的是,射频热凝治疗椎间盘仍有其局限性,如热凝的范围较小等。因此,作者通过靶点消融,这样针尖更靠近突出部位,效果更确切。与此同时,采用射频与其他技术的联合应用,以达到更好的疗效。
臭氧注射消融术是通过在靶点处注射少量高浓度的臭氧,迅速氧化髓核内蛋白多糖,直接使髓核原纤维基质和胶原纤维细胞脱水回缩,从而减轻对周围神经、血管的压迫发挥治疗作用。研究显示,臭氧还具有抗炎镇痛作用,可以消除髓核的化学性和免疫性炎症[17]。本资料结果显示患者术后1个月的优良率可达85.4%,术后6个月优良率为86.3%,且未有患者在治疗后发生严重并发症,提示CT引导下靶点射频联合臭氧注射消融术是治疗椎间盘突出症的良好方法,具有较高的安全性。与本资料不同,Chou等[18]研究认为,包括射频热凝在内的脊柱微创介入手术疗效有限,这可能与国内外对于椎间盘突出症的介入治疗多通过C型臂X线荧屏引导下治疗,定位不够精准有关。此外,有报道认为臭氧注射后可使软组织和骨性结构间有较多硬粘连而产生相应并发症[19],但Buric等[20]通过一项回顾性研究发现,臭氧注射对约75%的椎间盘突出症患者是安全和有效的,并能保持十年的效益。
[1] Mustafa Güler,Teoman Aydın,Erdal Akgöl,et al.Concomitance of fibromyalgia syndrome and cervical disc herniation.J Phys Ther Sci,2015,27:785-789.
[2] Lee JH,Kim JS,Lee JH,et al.Comparison of cervical kinematics between patients with cervical artificial disc replacement and anterior cervical discectomy and fusion for cervical disc herniation.Spine J,2014,14:1199-1204.
[3] Bonaldi G,Baruzzi F,Facchinetti A,et al.Plasma radio-frequencybased diskectomy for treatment of cervical herniated nucleus pulposus:feasibility,safety,and preliminary clinical results.AJNR Am J Neuroradiol,2006,27:2104-2111.
[4] Kapural L,Vrooman B,Sarwar S,et al.A randomized,placebocontrolled trial of transdiscal radiofrequency,biacuplasty for treatment of discogenic lower back pain.Pain Med,2013,14:362-373.
[5] Zhenhua Zeng,Min Yan,Yi Dai,et al.Percutaneous bipolar radiofrequency thermocoagulation for the treatment of lumbar disc herniation.J Clin Neurosci,2016,24:S0967-5868.
[6] Gangi A,Tsoumakidou G,Buy X,et al.Percutaneous techniques for cervical pain of discal origin.Semin Musculoskelet Radiol,2011,15:172-180.
[7] Alexandre A,Corò L,Azuelos A,et al.Intradiscal injection of oxygen-ozone gas mixture for the treatment of cervical disc herniations.Acta Neurochir Suppl,2005,92:79-82.
[8] Magalhaes FN,Dotta L,Sasse A,et al.Ozone therapy as a treatment for low back pain secondary to herniated disc:a systematic review and meta-analysis of randomized controlled trials.Pain Physician,2012,15:E115-129.
[9] Yu L,Song Y,Yang X,et al.Systematic review and metaanalysis of randomized controlled trials:comparison of total disk replacement with anterior cervical decompression and fusion.Orthopedics,2011,34:e651-658.
[10] Le H,Sandhu FA,Fessler RG.Clinical outcomes after m inimalaccess surgery for recurrent lumbar disc herniation.Neurosurg Focus,2003,15:El2.
[11] Baek SH,Oh JW,Shin JS,et al.Long term follow-up of cervical intervertebral disc herniation inpatients treated with integrated complementary and alternative medicine:a prospective case series observational study.BMC Complement Altern Med,2016,16:52.
[12] Gadjradj PS,van Tulder MW,Dirven CM,et al.Clinical outcomes after percutaneous transforaminal endoscopic discectomy for lumbar disc herniation:a prospective case series.Neurosurg Focus,2016,40:E3.
[13] Lee JH,Lee SH.Comparison of Clinical Efficacy Between Interlaminar and Transforaminal Epidural Injection in Patients With Axial Pain due to Cervical Disc Herniation.Medicine(Balt imore),2016,95:e2568.
[14] Wong JJ,Côté P,Quesnele JJ,et al.The course and prognostic factors of symptomatic cervical disc herniation with radiculopathy:a systematic review of the literature.Spine J,2014,14:1781-9.
[15] Fei Z,Fan C,Ngo S,et al.Dynamic evaluation of cervical disc herniation using kinetic MRI.J Clin Neurosci,2011,18:232-236.[16] Chen YC,Lee SH,Chen D.Intradiscal pressure study of percutaneous disc decompression with nucleoplasty in human cadavers.Spine,2003,28:661-665.
[17] Muto M,Andreula C,Leonardi M.Treatment of herniated lumbar disc by intradiscal and intraforaminal oxygen-ozone(O2-O3) injection.J Neuroradiol,2004,31:183-189.
[18] Chou R,Atlas SJ,Stanos SP,et al.Nonsurgical interventional therapies for low back pain:a review of the evidence for an American Pain Society clinical practice guideline.Spine,2009,34:1078-1093.
[19] Vanni D,Galzio R,Kazakova A,et al.Intraforaminal ozone therapy and particular side effects:preliminary results and early warning.Acta Neurochir(Wien),2016,158:491-496.
[20] Buric J,Rigobello L,Hooper D.Five and ten year follow-up on intradiscal ozone injection for disc herniation.Int J Spine Surg,2014,8:10.
Objective To summarize the treatment effectiveness and safety of radiofrequency thermocoagulation technology combined with intradiscal ozone injection under CT-guidance in the treatment of 542 cases with cervical disc herniation. Methods 542 patients with cervical disc herniation were involved in this study. Under the CT-guidance,these patients were treated by radiofrequency thermocoagulation technology combined with intradiscal ozone injection. Visual analogue scale(VAS)was adopted to evaluate the scores of pain and the clinical efficacy of this therapy was evaluated after the treatment. Results 24 hours to 6 months after the treatment,the efficacy rates were 85.9%,79.9%,85.4%,86.9% and 86.3%,respectively. VAS scores were significantly decreased from 24 hours to 6 months after the treatment when compared with that before operation(P<0.05). No serious complications were found in this fellow-up study. Conclusion Under CT-guidance,radiofrequency thermocoagulation technology combined with intradiscal ozone injection is an effective and minimally invasive therapy for the cervical disc herniation,which has a good safety record.
Radiofrequency thermocoagulation technology Intradiscal ozone injection Cervical disc herniation
浙江省医学会临床科研基金(2012ZYC-A66)
314100 浙江省嘉善县第一人民医院(曾振华 戴仪邓硕 邹三宝 尹君)
310000 浙江大学附属第二医院(严敏)



