李家瑞张红燕尚跃丰曹书华
社区获得性肺炎伴发急性肾损伤的预后危险因素分析
李家瑞1张红燕2尚跃丰1曹书华3
目的 探讨社区获得性肺炎(CAP)患者伴发急性肾损伤(AKI)的预后危险因素。方法456例CAP患者为无伴发AKI(N-AKI)组和伴发AKI组。AKI组又根据RIFLE的严重程度级别分为3个亚组:危险(Risk)、损伤(Injury)和衰竭(Failure)组。比较各组患者CAP的严重程度,各项临床指标和预后评估指标的差别;多因素分析采用Logistic回归模型,生存分析采用Kaplan-Meier法,分析影响CAP患者预后不良的危险因素及RIFLE标准在预后评估中作用。结果456例CAP患者中有30%(135例)伴发AKI,诊断为Risk 61例(45.2%),Injury 23例(17%),Failure 51例(37.8%)。CAP患者PSI评分为Ⅰ~Ⅲ级的患者(300例)中有23.3%(70例)伴发AKI,PSI分级≥IV的患者(156例)中有41.7%(65例)伴发AKI,差异有统计学意义(P<0.01)。伴发AKI的CAP患者30 d病死率随AKI严重程度增加(N-AKI患者6.2%,Risk患者14.8%,Injury患者21.7%,Failure患者45.1%)。此外,随着AKI严重程度增加,需要机械通气、正性肌力药物和肾脏替代治疗的患者比例增加。Logistic回归分析显示合并AKI、>75岁、合并肾外器官衰竭是住院CAP患者预后不良的危险因素。结论住院CAP患者伴发AKI的预后不良。RIFLE诊断及分级标准可有效评估CAP伴发AKI患者的预后。
社区获得性肺炎;急性肾损伤;RIFLE分级;预后;危险因素
社区获得性肺炎(community acquired pneumonia,CAP)被定义为医院外罹患的感染性肺部炎症,具有明显潜伏期的病原体感染,而在入院后平均潜伏期内发病的肺炎也属于CAP的范畴[1]。文献报道CAP是威胁人类健康的重要疾病,患病率约占人群的12%。我国每年约有250万CAP患者,死于CAP的患者超过12万人[2]。急性肾损伤(acute kidney injury,AKI)是指不超过3个月的肾脏功能或结构方面的异常,包括血、尿、组织检测或影像学方面的肾损伤标志物的异常[3],其发病率呈上升趋势,国内有报道以肌酐(SCr)短时间上升≥50%作为入选标准,住院患者AKI的发病率为8.46%[4]。在校正年龄、性别等因素后,AKI是住院患者死亡的独立危险因素,增加住院患者4倍的死亡风险。研究发现CAP住院患者是伴发AKI的高危人群[5-6],而有关AKI在CAP患者中的发生情况及其对CAP患者预后影响的研究甚少。因此,本研究拟探讨CAP患者伴发AKI的临床特点及其对住院CAP患者预后评估的影响因素。
1 对象与方法
1.1 研究对象及分组 为我院2009年12月—2013年3月收治的CAP患者456例,其中男250例,女206例,年龄40~80岁,平均(66.3±5.8)岁。入选标准如下:符合2006年中华医学会呼吸病学分会制定的CAP诊断标准,且年龄≥18岁,住院前接受或未接受抗感染治疗,收住重症监护病房(ICU)或普通病房。排除标准:(1)医院获得性肺炎(入院48 h后在医院内发生的肺炎,也包括出院后48 h内发生的肺炎)。(2)既往存在慢性肾脏疾患、肾功能异常或正在接受肾脏替代治疗(腹膜透析或血液透析)。(3)胸腔恶性肿瘤。(4)正在服用免疫抑制药物(环孢素等)。(5)肺栓塞。根据是否发生AKI分为2组,无伴发AKI(N-AKI)组和伴发AKI组。本研究经患者或家属知情同意,并经医院伦理委员会批准。
1.2 研究方法
1.2.1 AKI的诊断及分级 根据AKI∕ARF的RIFLE分级诊断标准[5],AKI∕ARF严重程度分为3个亚组:包括危险(Risk)、损伤(Injury)、衰竭(Failure);2个预后级别:肾功能丧失(Loss),终末期肾病(end stage renal disease,ESRD),见表1。为避免扩大假阳性结果,本研究以本院Scr正常参考值上限为基础值,即男性12 mg∕L,女性10 mg∕L;肾小球滤过率(GFR)以男性100 mL∕min,女性90 mL∕min为基础值。
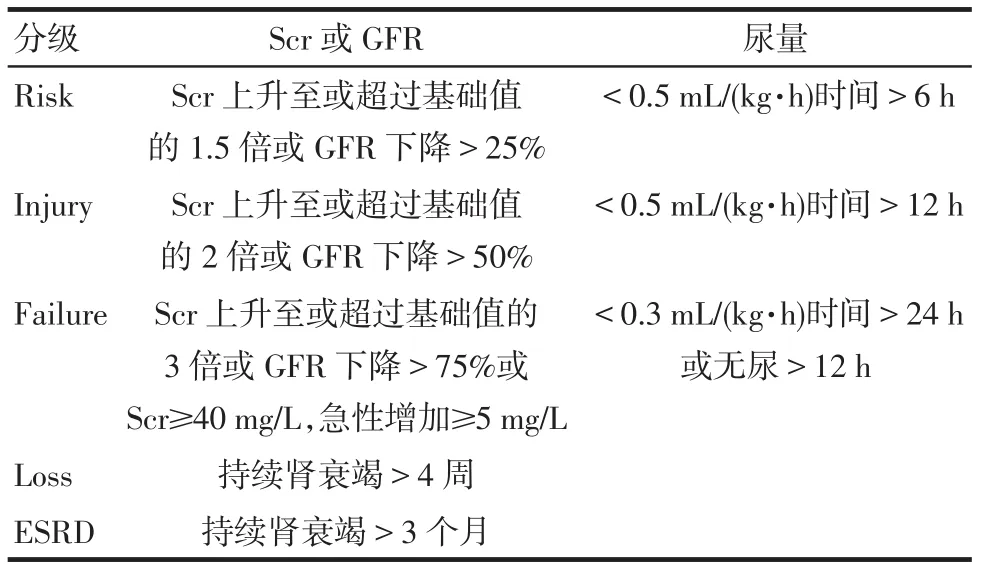
Tab.1 The RIFLE diagnostic criteria of AKI/ARF表1 AKI/ARF的RIFLE分级诊断标准
1.2.2 CAP的病情评估 根据2006年中华医学会呼吸病分会制定的《社区获得性肺炎诊断和治疗指南》病情评估标准和肺炎严重程度指数(Pneumonia Severity Index,PSI)评分系统对CAP患者的病情进行评估。
1.2.3 数据采集与分析 收集以下数据:年龄,性别,基础疾病,体格检查参数包括意识状态、体温、呼吸频率、脉搏、血压、心率及Scr等实验室指标;治疗情况及预后;预后指标包括30 d病死率,是否需要机械通气、正性肌力药物支持、肾脏替代治疗(血液透析或腹膜透析)、住院天数及合并肾外器官损伤(或衰竭)情况等。
1.3 统计学方法 采用SPSS 13.0软件进行统计学分析。符合正态分布的计量资料用均数±标准差(±s)表示,2组间比较采用两独立样本的t检验;多组间比较采用ANOVA方差分析。计数资料2组或多组间比较采用卡方(χ2)检验,当存在1个及以上单元格理论频数小于1时,采用Fisher精确概率法。多因素分析采用Logistic回归模型。生存分析采用Kaplan-Meier法。P<0.05为差异有统计学意义。
2 结果
2.1 CAP伴发AKI的发生情况 456例CAP患者中有135例(30%)伴发AKI。根据RIFLE的诊断标准,61例(45.2%)诊断为Risk,23例(17%)诊断为Injury,51例(37.8%)诊断为Failure。根据PSI评分标准,PSI评分为Ⅰ~Ⅲ级的患者(300例)中有70例(23.3%)伴发AKI,PSI评分≥Ⅳ的患者(156例)中有 65例(41.7%)伴发 AKI,差异有统计学意义(χ2=15.655,P<0.01)。
2.2 伴发AKI患者预后评估 按照RIFLE的诊断标准分组,4组CAP患者30 d病死率、需要机械通气的比例、正性肌力药物的使用比例、接受肾脏替代治疗的患者比例和住院天数比较差异均有统计学意义(P<0.01),随着伴发AKI的严重程度增加,各观察指标均呈现依次递增的趋势,见表2。
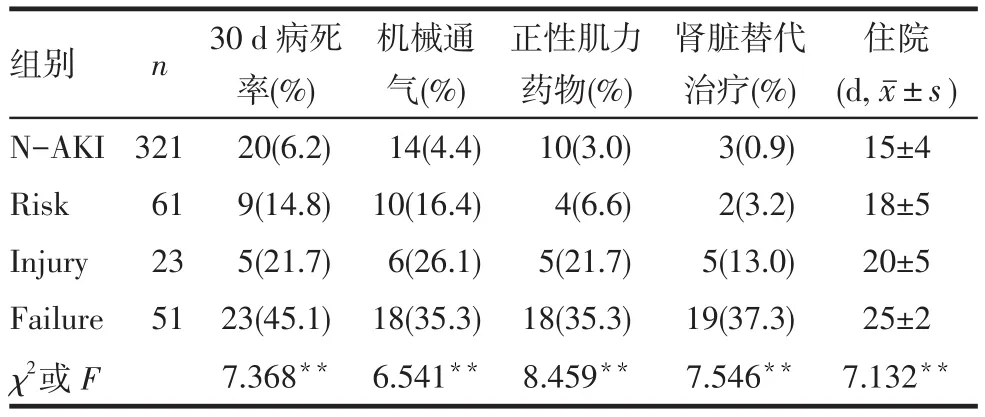
Tab.2 Prognostic evaluation of CAP patients accompanied with AKI and Non-AKI表2 无急性肾损伤患者和伴发急性肾损伤患者预后评估
2.3 影响CAP患者预后的因素分析 以CAP患者30 d内是否存活为因变量(存活=0,死亡=1),筛选有临床意义的指标分别进行赋值,进行Logistic回归分析,自变量及赋值分别为年龄(40~59岁=0,60~75岁=1,>75岁=2),合并AKI(否=0,是=1),合并肾外器官衰竭(否=0,是=1),APECHEⅡ评分(<20= 0,≥20=1)、是否抗凝治疗(否=0,是=1),机械通气(否=0,是=1),正性肌力药物(否=0,是=1),肾脏替代治疗(否=0,是=1)及合并真菌感染(否=0,是=1),最终年龄、合并AKI和合并肾外器官衰竭进入回归模型,结果显示年龄>75岁、合并AKI、合并肾外器官衰竭是住院CAP患者预后不良的危险因素,见表3。
2.4 生存分析 对4组CAP患者30 d生存情况进行分析,结果显示:Failure组患者生存率显着低于Injury组、Risk组及N-AKI组(Log-rank χ2分别为7.378、9.861、11.572,均P<0.05);Injury组患者生存率低于N-AKI组(Log-rank χ2=8.356,P<0.05);Risk组患者生存率和N-AKI组差异无统计学意义(Log-rank χ2=2.356,P=0.15),见图1。
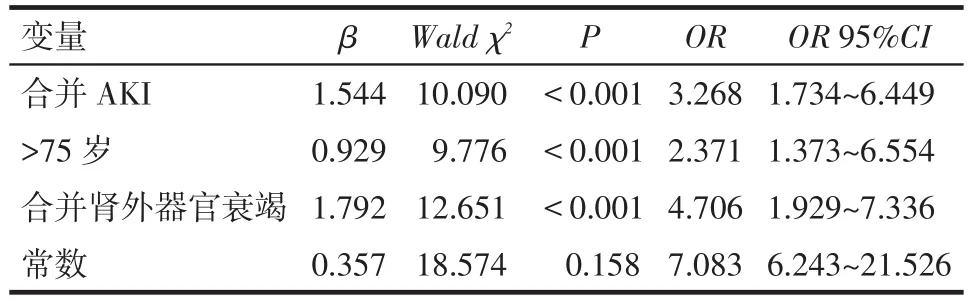
Tab.3 Multiple factors Logistic regression analysis of prognosis in CAP patients表3 CAP患者预后多因素Logistic回归分析
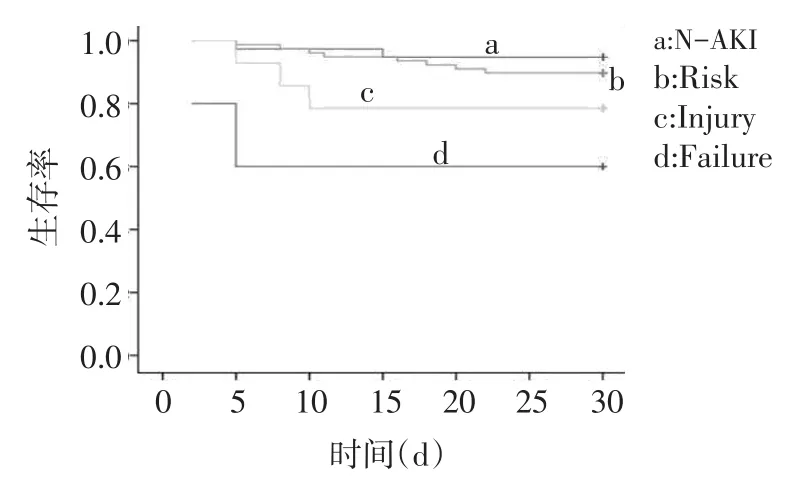
Fig.1 Survival analysis图1 生存分析
3 讨论
CAP是常见的感染性疾病,文献报道5%的住院患者会伴发AKI,ICU患者有更高的AKI发病率(6%~23%)[7],也被认为是CAP的常见并发症[8];Murugan等[9]发现AKI在CAP患者中很常见,34% 的CAP患者会伴发AKI,25%的非重症CAP患者发生AKI。在我国关于AKI在CAP患者中的发生情况和对CAP预后评估的研究报道较少。本组资料显示456例CAP患者中有30%(135例)伴发AKI。
本组资料显示,CAP患者伴发AKI的30 d病死率较单纯CAP患者明显增高;生存分析显示,4组CAP患者中,伴发AKI的Failure组生存率最低,NAKI组生存率最高;多因素分析结果也显示了合并AKI、>75岁和合并肾外器官衰竭是CAP患者预后不良的危险因素;上述结果说明,伴发AKI的CAP患者预后不良。此外,本研究还显示了合并AKI的CAP患者30 d病死率随着RIFLE分级标准级别的增加而增加,且住院天数明显增加,需要机械通气、正性肌力药物和肾脏替代治疗的患者也同样增加。因此,RIFLE的诊断和分级标准有利于对合并AKI的CAP患者进行预后评估。既往的研究证实,ICU重症AKI患者中,RIFLE的分级标准严重性增加会增加患者的病死率,而这些患者肾脏的损伤会进一步恶化[10]。这些研究支持AKI患者极其需要早期诊断和早期干预,阻止病情进一步的恶化。本研究中CAP患者中AKI的发生率约为30%,PSI评分为Ⅰ~Ⅲ级患者中AKI的发病率为23.3%,PSI≥Ⅳ患者为41.7%,该结果提示必须重视CAP患者AKI的发生,包括非重症肺炎的患者。AKI和急性肺损伤(acute lung injury,ALI)均是ICU危重症患者的严重情况,二者相互作用,AKI的出现常会造成远隔器官(尤其肺)的损伤,使病情更趋复杂和进一步恶化[11]。
本研究存在某些局限性,如样本量小、为单中心临床观察,对CAP伴发AKI的RIFLE分级标准是按照患者入院时血肌酐和GFR水平诊断的,忽略了在住院过程中发生的AKI和肾功能进一步恶化的情况;此外,本研究阐述了合并AKI的CAP患者仅采用RIFLE标准来分析CAP和AKI之间的关系及其对预后的评估作用;将来有必要进行大样本、多中心,基于AKI的RIFLE标准、AKIN(Acute kidney injury network)标准和2012年KDIGO(Kidney disease improving global outcomes)的AKI临床实践指南标准的深入对比研究。
总之,住院CAP患者部分合并AKI,且伴发AKI的患者预后不良,临床工作中应重视CAP患者AKI的发生情况和器官(肺、肾等)之间的交互作用,早期诊断和治疗将有助于改善患者预后。
[1]Wu C,Rosenfeld R,Clermont G.Using data-driven rules to predict mortality in severe community acquired pneumonia[J].PLoS One,2014, 9(4):e89053.
[2]Liu YN,Chen MJ,Zhao TM,et al.A multicentre study on the pathogenic agents in 665 adult patients with community-acquired pneumonia in cities of China[J].Chinese Journal of Tuberculosis and Respiratory Diseases,2006,29(1):3-8.
[3]Murugan R,Weissfeld L,Yende S,et al.Association of statin use with risk and outcome of acute kidney injury in community-acquired pneumonia[J].Clin J Am Soc Nephrol,2012,7(6):895-905.
[4]Qiu L,Chen LM,Li XM,etal.Survey of acute kidney injury in hospitalizedpatients[J].Chinese Journal of LaboratoryMedicine,2009,32 (1):46-50.[邱玲,陈丽萌,李雪梅,等.住院患者急性肾损伤的发病情况调查[J].中华检验医学杂志,2009,32(1):46-50.]
[5]Akram AR,Singanayagam A,Choudhury G,et al.Incidence and prognostic implications of acute kidney injury on admission in patients with community-acquired pneumonia[J].Chest,2010,138(4):825-832.
[6]Cavallazzi R,Wiemken T,Ramirez J.Risk factors for pulmonary tuberculosis in community-acquired pneumonia[J].Eur Respir J,2014, 43(4):1214.
[7]Daher EF,Marques CN,Lima RS,et al.Acute kidney injury in an infectious disease intensive care unit-an assessment of prognostic factors[J].Swiss Med Wkly,2008,138(9-10):128-133.
[8]Remington LT,Sligl WI.Community-acquired pneumonia[J].Curr Opin Pulm Med,2014,20(3):215-224.
[9]Murugan R,Karajala-Subramanyam V,Lee M,et al.Genetic and Inflammatory Markers of Sepsis GenIMS Investigators.Acute kidney injury in non-severe pneumonia is associated with an increased immune response and lower survival[J].Kidney Int,2010,77(6):527-535.
[10]Hoste EA,Clermont G,Kersten A,et al.RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients:a cohort analysis[J].Crit Care,2006,10(3):R73.
[11]Santiago AI,Belzunegui OT.Variation of the characteristics and epidemiology of patients with pneumonia acquired in the community treated in hospital A and E services[J].An Sist Sanit Navar,2014,37 (1):139-145.
(2014-04-27收稿 2014-07-04修回)
(本文编辑 李国琪)
Analysis of Prognostic Risk Factors in Patients with Community Acquired Pneumonia Complicated with Acute Kidney Injury
LI Jiarui1,ZHANG Hongyan2,SHANG Yuefeng1,CAO Shuhua3
1 Department of Emergency Medicine,Tianjin Hospital,Tianjin 300211,China;2 Department of Hemodialysis center,Tianjin Hospital;3 Tianjin First Center Hospital,Tianjin.
ObjectiveTo explore clinical characteristics and prognostic risk factors in patients with community acquired pneumonia(CAP)complicated with acute kidney injury(AKI).MethodsIn total,456 CAP patients were included based on the diagnostic guide.According to whether the patients were accompanied with AKI,the patients were divided into two groups(non-AKI group and AKI group).AKI group were further divided into risk group,injury group and failure group by RIFLE criteria using admission creatinine.Severity in CAP patients,clinical indexes and prognostic evaluation indexes were compared between different groups.Multiple factors were analyzed using Logistic regression model,survivalanalysis were examined by Kaplan-Meier,which analyzed the risk factors of poor prognosis in CAP patients and the role of RIFLE criteria in prognostic evaluation.ResultsThirty percent(135)of the total 456 CAP patients were accompanied with AKI.Patients in AKI group were further divided into risked group(45.2%,61 patients),injury group(17%,23 patients)and failure group(37.8%,51 patients)according to the RIFLE diagnostic criteria using basal creatinine level.Among the 300 patients with PSI gradeⅠtoⅢ,23.3%(70)of patients developed AKI while among 156 patients who are with PSI gradeⅣor over,65 patients(41.7%)developed AKI(P<0.01).The 30-day mortality of CAP patients accompanied with AKI were increased compared to Non-AKI group(Non-AKI:6.2%;Risk:14.8%;Injury:21.7%;Failure:45.1%).With deteriorating in RIFLE criteria,the portion of patients who required mechanical ventilation,inotropic support(MV∕IS)and renal replacement therapy(RRT)increased too.Logistic analysis revealed that AKI,age of 75 years or older and extra-renal organ failure were the risk factors of poor prognosis in patients with CAP.The rate of survivors was decreased in the CAP patients accompanied with AKI compared with those who did not.ConclusionThere is certain incidence of AKI to complicate CAP patients who will have a poor prognosis.RIFLE diagnostic criteria is a valuable tool to evaluate prognosis of CAP patients complicated with AKI.
community acquired pneumonia;acute kidney injury;RIFLE class;prognosis;risk factors
R563.1,R692
A
10.3969∕j.issn.0253-9896.2014.10.014
天津市医药卫生重点学科攻关项目(10kg118)
1天津市天津医院急诊医学科(邮编300211),2血液透析中心;3天津市第一中心医院急救医学研究所



