程炳娟,刘戈力,李宁,杨箐岩,郑荣秀
特发性矮小生长激素受体外显子3基因多态性与生长激素轴的关系
程炳娟1,刘戈力2△,李宁3,杨箐岩2,郑荣秀2
摘要:目的探讨生长激素受体(GHR)外显子3基因型与特发性矮小(ISS)患者生长激素-胰岛素样生长因子-胰岛素样生长因子结合蛋白(GH-IGFs-IGFBPs)轴的关系。方法选取108例ISS儿童,提取外周血DNA并采用多重PCR法进行GHR外显子3基因分型,根据基因型结果分为GHRfl组和GHRd3组。测量2组身高、体质量,并计算体质指数(BMI)及BMI标准差计分(SDS);测定空腹胰岛素样生长因子(IGF)-1、胰岛素样生长因子结合蛋白(IGFBP)-3,计算IGF-1 SDS、IGFBP3 SDS;同时进行生长激素激发试验,测定血清GH峰值。108例中选取55例自愿接受重组人生长激素[rhGH,0.15 IU/(kg·d)]治疗3个月,分析基因型与rhGH治疗后IGF-1水平的关系。结果108例ISS中GHRfl 63例,GHRd3 45例。2组间BMI、IGF-1、IGFBP3、GH峰值以及IGF-1 SDS、IGFBP3 SDS差异均无统计学意义(均P > 0.05);多元逐步回归分析示年龄、IGFBP3、lg(BMI)、lg(GH峰值)是lgIGF-1的影响因素(均P < 0.05);55例接受rhGH治疗ISS中GHRd3组(34例)IGF-1和IGF-1 SDS治疗前后差值(△IGF-1,△IGF-1 SDS)高于GHRfl组(21例)。结论ISS儿童GHR外显子3基因多态性可能与IGF-1及IGFBP3水平无关,与GH敏感性有关。
关键词:特发性矮小;受体,促生长素;基因多态性;胰岛素样生长因子-1;胰岛素样生长因子结合蛋白-3;体质指数
GH)和生长激素受体(growthhormone receptor,
GHR)结合信号转导通路中因子的基因多态性有关。GH与GHR结合后可通过JAK2/STAT5信号转导通路激活胰岛素样生长因子基因转录,调节线性生长和代谢[1]。由于GHR基因外显子3全长型(GHR exon 3 full-length,GHRfl)内在的长末端重复序列重组,导致GHR基因外显子3存在多态性[2]。
这种常见的多态性导致GHR细胞外区域23个残基和糖基化位点的丢失,由此造成的GHR基因3缺失型(GHR exon 3 -deleted,GHRd3)多态性不会影响
GH与GHR结合,而是与异常的生长激素-胰岛素样生长因子-胰岛素样生长因子结合蛋白(GHIGFs-IGFBPs)轴有关[3]。有研究认为GHR基因多态性可影响血清胰岛素样生长因子-1( insulin-like growth factor -1,IGF-1)水平,从而影响生长轴的功能,可能是部分ISS发病的危险因素[4]。本文主要探究特发性矮小儿童GHR外显子3基因多态性与
IGF-1、IGFBP3及GH敏感性的关系。
1 对象与方法
1.1研究对象选取2014年6月—2015年6月在天津医科大学总医院儿科内分泌门诊就诊的108例ISS儿童。男61例,女47例,年龄3~15岁,中位年龄8.2岁。入选标准:(1)身高低于同年龄同性别正常儿童标准身高2个标准差或第3百分位数。(2)GH激发试验中,GH峰值>7.0mg/L[5]。(3)血常规、甲状腺功能、肝肾功能、血糖、胰岛素、电解质检查均无异常。(4)出生体质量及身长在正常范围内。(5)排除其他遗传代谢病、染色体异常、先天性骨骼异常和慢性疾病。(6)头颅下丘脑垂体区未见异常。108例ISS儿童中,55例愿意接受重组人生长激素(rhGH)治疗,其中男29例,女26例,年龄3~14岁,中位年龄9岁。
1.2主要试剂及仪器全基因组DNA快速提取试剂盒(离心柱型)、PCRmasterMix、扩增引物均购自北京百泰克生物技术有限公司;IGF-1、IGFBP3、GH配套试剂及immulite 2000化学发光免疫分析仪均购自SIMENS公司;盐酸可乐定(75 μg/片)购自常州制药厂有限公司;溴吡斯的明(60mg/片)购自上海三维长江制药厂;rhGH(30 IU/支)购自长春金赛药业有限责任公司。
1.3方法
1.3.1GHR外显子3基因多态性检测收集108例ISS儿童全血标本,提取淋巴细胞中DNA。根据参考文献[2]采用多重PCR法检测GHR外显子3基因多态性。PCR上游引物G1:5′-TGTGCTGGTCTGTTGGTCTG-3′;下游引物G2:5′-AGTCGTTCCTGGGACAGAGA- 3′;G3:5′- CCTGGATTAA⁃CACTTTGCAGACTC-3′。PCR反应体系:2×Mastermix 25 μL,上、下游引物(10 μmoL)各2 μL,模板DNA 5 μL,补蒸馏水至总体积50 μL。反应条件:94℃5min;94℃30 s,60℃30 s,72℃90 s;72℃延长7min,35个循环。PCR产物经1%琼脂糖凝胶电泳分离并判定其基因型。GHR外显子3存在fl/fl(无外显子3缺失的纯合子),fl/d3(有一条染色体缺失外显子3的杂合子)以及d3/d3(2条染色体都缺失外显子3的纯合子)3种基因型。GHR fl和GHR d3长度分别为935 bp和532 bp。为避免假性纯合子GHR d3,每个d3/d3基因型进行第2次PCR确保实验准确性[6]。
1.3.2临床及生化指标测定测量108例ISS儿童身高和体质量,计算体质指数(BMI),为消除性别及年龄的影响,同时BMI标准差计分(SDS)[7-8]。空腹取肘正中静脉血1次,测定IGF-1和IGFBP3水平,并根据同性别、同年龄健康儿童参考值计算IGF-1 SDS[9]、IGFBP3 SDS[10],剩余样本用于后续实验。
1.3.3生长激素激发试验108例患儿口服相应剂量的溴吡斯的明(1mg/kg,最大量60mg)和盐酸可乐定(4 μg/kg,最大量150 μg),分别于给药后30min,60min,90min各取1次血,测定其GH水平,取最高值作为GH峰值。
1.3.4rhGH治疗后IGF-1水平测定55例自愿接受rhGH治疗的患儿每晚睡前皮下0.15 IU/(kg·d)注射1次,3个月后空腹取血测定IGF-1,并计算IGF-1差值(△IGF-1)及IGF-1差值SDS (△IGF-1 SDS)。
1.4统计学方法采用SPSS 20.0进行统计学分析。所有资料均通过Shapiro-Wilk test进行正态性检验,正态分布计量资料采用均数±标准差(±s)表示,组间比较采用t检验;偏态分布资料采用M(P25,P75)表示,组间比较采用Mann-Whit⁃ney U检验。计数资料采用例(%)表示,Hardy-Weinberg平衡检验采用卡方检验,回归分析采用多重线性回归分析。P < 0.05为差异有统计学意义。
2 结果
2.1基因多态性结果GHR基因外显子3基因多态性结果见图1。108例患者中,基因型fl/fl、fl/d3、d3/d3分别为63、38、7例,符合Hardy-Weinberg平衡(χ2=0.170,P > 0.05),提示本研究所选择人群代表性较好,能代表ISS人群一般情况。

Fig.1 Agarose gel electrophoresis of GHR exon 3图1 GHR外显子3琼脂糖凝胶电泳图
2.2临床生化指标比较将108例患儿按照基因型分为GHRfl组(63例)和GHRd3组(45例)。2组间年龄、性别、BMI、GH峰值、IGF-1、IGFBP3差别均无统计意义;将BMI、IGF-1、IGFBP3转换为SDS后,差异同样无统计学意义,见表1。

Tab.1 Comparison of clinical and biochemical parameters between two groups表1 各组间临床和生化指标的比较
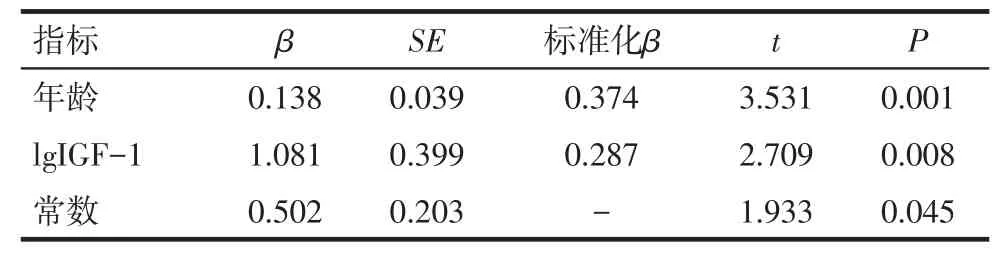
2.3IGF-1、IGFBP3值的多元逐步回归分析将非正态分布的IGF-1、GH峰值、BMI数据进行lg转换为正态分布,以年龄、lgGH峰值、lgBMI、IGFBP3、GHR外显子3基因型为自变量,lgIGF-1为因变量进行逐步多元回归分析。结果显示年龄、IGFBP3、 lgGH峰值、lgBMI是IGF-1的影响因素,GHR外显子3基因型因素被排除,见表2。以年龄、lgGH峰值、lgBMI、lgIGF-1、GHR外显子3基因型为自变量,IGFBP3为因变量进行逐步多元回归分析,结果显示只有年龄和IGF-1是IGFBP3的影响因素,见表3。

Tab.2 Multiple stepwise regression analysis of influencing factors of IGF-1 level in children of ISS表2 ISS患儿IGF-1水平影响因素的多重逐步回归分析
Tab.3 Multiple stepwise regression analysis of influencing fctors of IGFBP3 level in children of ISS表3 ISS患儿IGFBP3水平影响因素的多重逐步回归分析
2.4GH治疗后IGF-1水平变化55例ISS患者基因型fl/fl、fl/d3、d3/d3分别为34、18、3例,符合Hardy- Weinberg平衡(χ2=0.08,P > 0.05),分为GHRfl组(34例)和GHRd3组(21例)。2组间年龄、性别、基础IGF-1及IGF-1 SDS差异无统计学意义。经rhGH治疗后,GHRd3组△IGF-1、△IGF-1 SDS高于GHRfl组(P < 0.05),见表4。

Tab.4 IGF-1 response to GH treatment in two groups表4 2组间IGF-1对rhGH治疗反应
3 讨论
GH-IGFs-IGFBPs轴是调节儿童生长发育中最重要的神经内分泌轴。GH的促生长作用由IGF系统介导,它包括IGFs、IGFBPs、IGF受体及通过GH直接作用的IGF独立效应。IGF-1的生物学作用广泛,可促进细胞的生长、分化、成熟,并可抑制细胞凋亡,介导GH对机体的促生长作用[11]。IGFBP3是人体内IGF-1主要载体蛋白,受IGF-1水平的调控。IGFBP3与IGF-1结合后,能够维持IGF-1水平恒定,两者可作为评估生长失调的指标。本研究中笔者评估了可能与GHRd3基因型有关的GH轴相关因子及临床指标,以及rhGH治疗后IGF-1的水平变化。发现GHRfl组基础IGF-1 SDS、IGFBP3 SDS 与GHRd3组差异无统计学意义,与Ballerini等[4]研究结果一致,表明GHR外显子3基因多态性对基础IGF-1、IGFBP3生成无影响。多重逐步回归分析也同样显示GHR外显子3基因型不是基础IGF-1、IGFBP3生成的影响因素。
有报道指出42% ISS患儿BMI低于正常,且低BMI ISS表现为一定程度的IGF-1抵抗[12-13]。本研究显示BMI是IGF-1影响因素之一,考虑BMI与IGF-1抵抗可能存在关系。BMI是营养状况一个相对的总指标,可以解释GH治疗后的IGF-1水平差异[13]。ISS患者的rhGH治疗剂量是通过体质量计算的,同时需将IGF-1水平考虑在内。在低BMI ISS患儿中,为了减少以体质量为基础计算的生长激素剂量的负性影响,rhGH剂量应该根据体表面积计算,即使调整计算方法,低BMI ISS儿童每日rhGH剂量也会轻微低于正常BMI ISS儿童的剂量。
本研究中55例ISS儿童经3个月rhGH治疗后IGF-1 SDS均有增长,GHRd3组明显高于GHRfl组,提示对GH不敏感可能是ISS的病因之一。IGF-1是GH作用线性生长的主要调节因子,在rhGH治疗后IGF-1水平的增加是生长反应的一个标志[14]。体外研究表明,转染GHRd3型基因的人胚胎肾细胞比GHRfl型基因的转录活性更高[15]。遗传药理学研究也发现GHRd3型ISS患者对rhGH治疗疗效较好[15-16]。另有研究提出在ISS儿童IGF-1激发试验中,GHRd3基因型患儿IGF-1升高更加明显,支持GHRd3基因型较GHRfl基因型ISS对GH敏感性高[17]。但Hellgren等[18]发现ISS患者在rhGH治疗初期,GHRfl组与GHRd3组IGF-1 SDS没有区别,而GHRfl组中基础IGFBP3水平低于GHRd3组,且经过1年的rhGH治疗后,IGF-1 SDS和IGFBP3 SDS的增加在2组中均无明显差别。本研究只观察3个月rhGH治疗疗效,由于时间较短,并未对身高作评估分析,仍需长期观察GH治疗后IGF-1变化及身高增长与基因型的关系。同时由于本研究样本量相对较少,今后有待扩大样本深入研究。
参考文献
[1] David A,hwa V,metherell LA, et al.Evidence for a continuum of genetic, phenotypic, and biochemical abnormalities in children with growthhormone insensitivity[J].Endocr Rev, 2011,32(4):472-497.doi: 10.1210/er.2010-0023.
[2] Pantel J,machinis K, SobriermL, et al.Species-specific alternative splicemimicry at the growthhormone receptor locus revealed by the lineage of retroelements during primate evolution[J].J Biol Chem, 2000,275(25):18664-18669.doi: 10.1074/jbc.M001615200.
[3] El KM,mella P, Rashadm, et al.Growthhormone/IGF-I axis and growthhormone receptormutations in idiopathic short stature[J].Horm Res Paediatr, 2011,76(5):300-306.doi: 10.1159/000330191.
[4] BallerinimG, DomenehM, Scaglia P, et al.Association of serum components of the GH-IGFs-IGFBPs system with GHR-exon 3 polymorphism in normal and idiopathic short stature children[J].Growthhorm IGF Res, 2013,23(6):229- 236.doi: 10.1016/j.ghir.2013.08.003.
[5] Cohen P, Germak J, Rogol AD, et al.Variable degree of growthhor⁃mone (GH) and insulin-like growth factor (IGF) sensitivity in chil⁃dren with idiopathic short stature compared with GH-deficient pa⁃tients: evidence from an IGF-based dosing study of short children [J].J Clin Endocrinolmetab, 2010,95(5):2089-2098.doi: 10.1210/jc.2009-2139.
[6] Audi L, Esteban C, Carrascosa A, et al.Exon 3-deleted/full-length growthhormone receptor polymorphism genotype frequencies in Spanish short small-for-gestational-age (SGA) children and adoles⁃cents (n=247) and in an adult control population (n=289) show in⁃creased fl/fl in short SGA[J].J Clin Endocrinolmetab, 2006,91(12): 5038-5043.doi:http://dx.doi.org/10.1210/jc.2006-0828.
[7] Cole TJ, Freeman JV, PreecemA.Bodymass index reference curves for the UK, 1990[J].Arch Dis Child, 1995,73(1):25-29.doi: 10.1136/adc.73.1.25.
[8] Zhang YQ, Lih, Ji CY, et al.Bodymass index growth curves for Chinese children and adolescents 0- 18 years[J].Chin J Pediatr, 2009,47(7):493.[张亚钦,李辉,季成叶,等.中国0一18岁儿童、青少年体块指数的生长曲线[J].中华儿科杂志, 2009,47(7):493].
[9] Isojima T, Shimatsu A, Yokoya S, et al.Standardized centile curves and reference intervals of serum insulin-like growth factor-I (IGFI) levels in a normal Japanese population using the LMSmethod[J].Endocr J, 2012,59(9): 771-780.
[10] Guven B, Canm,mungan G, et al.Reference values for serum levels of insulin-like growth factor 1 (IGF-1) and IGF-binding protein 3 (IGFBP-3) in the West Black Sea region of Turkey[J].Scand J Clin Lab Invest, 2013,73(2):135-140.doi: 10.3109/00365513.2012.755739.
[11] Xia JJ, Zheng XY, Li LM, et al.Correlation between atherogenic in⁃dex of plasma level andmetabolism components in adult growthhor⁃mone deficiency patients[J].Med J Chin PLA, 2014,39(12):975-980.[夏佳佳,郑晓雅,李林蔓,等.成人生长激素缺乏症患者血浆致动脉粥样硬化指数与代谢组分变化的相关性分析[J].解放军医学杂志, 2014, 39 (12):975-980].doi: 10.11855/j.issn.0577-7402.2014.12.10.
[12] Cengiz P, Bas F, Atalar F, et al.Growthhormone/insulin- like growth factor-1 axis as related to bodymass index in patients with idiopathic short stature[J].J Clin Res Pediatr Endocrinol, 2013,5(1): 13-19.doi: 10.4274/Jcrpe.901.
[13] Roman R, Iniguez G, Lammoglia JJ, et al.The IGF-I response to growthhormone is related to bodymass index in short children with normal weight[J].Horm Res, 2009,72(1):10- 14.doi: 10.1159/000224335.
[14] Cohen P, Rogol AD, Weng W, et al.Efficacy of IGF-based growthhormone (GH) dosing in nonGH-deficient (nonGHD) short stature children with low IGF-I is not related to basal IGF-I levels[J].Clin Endocrinol (Oxf), 2013,78(3):405-414.doi: 10.1111/cen.12014.
[15] Dos SC, Essioux L, Teinturier C, et al.A common polymorphism of the growthhormone receptor is associated with increased respon⁃siveness to growthhormone[J].Nat Genet, 2004,36(7):720-724.doi: 10.1038/ng1379.
[16] Jorge AA, Arnhold IJ.Growthhormone receptor exon 3 isoforms and their implication in growth disorders and treatment[J].Horm Res, 2009,71( Suppl 2):55-63.doi: 10.1159/0001924 38.
[17] ToyoshimamT, Castroneves LA, Costalonga EF, et al.Exon 3-delet⁃ed genotype of growthhormone receptor (GHRd3) positively influ⁃ences IGF-1 increase at generation test in children with idiopathic short stature[J].Clin Endocrinol (Oxf), 2007,67(4):500-504.
[18]hellgren G, Glad C A, Jonsson B, et al.The growthhormone recep⁃tor exon 3- deleted/full- length polymorphism and response to growthhormone therapy in prepubertal idiopathic short children[J].Growthhorm IGF Res, 2015,25(3):127- 135.doi: 10.1016/j.ghir.2015.02.003.
(2015-07-06收稿2015-09-09修回)
(本文编辑胡小宁)
读者·作者·编者
Association of serum components of GH axis with GHR exon 3 polymorphism in idiopathic short stature children
CHENG Bingjuan1, LIU Geli2△,LI Ning3, YANG Jingyan2, ZHENG Rongxiu2
1 Graduate School of Tianjinmedical University, Tianjin 300070, China; 2 Department of Pediatric, 3 Department of Nuclearmedicine Laboratory, Generalhospital of Tianjinmedical University△Corresponding Author E-mail: liugeli2001@126.com
Abstract:Objective To investigate the possible association of circulating components of GH-IGFs-IGFBPs system with the GHR-exon 3 genotype in idiopathic short stature (ISS) children.Methods Genomic DNA was extracted and isolat⁃ed from peripheral leukocytes in 108 ISS children.GHR-exon 3 polymorphism was analyzed withmultiplex poly-merase chain reactions (PCR) assay.According to the results of genotype, ISS children were divided into GHRfl group and GHRd3 group.Theheight and weight were recorded in two groups.The bodymass index (BMI) and BMI standard deviation score (SDS) weremeasured.The serum levels of insulin-like growth factor (IGF) -1, IGF-binding protein (IGFBP)-3, IGF-1 SDS and IGFBP3 SDS were calculated.GH stimulation test was used tomeasure the serum GH peak value.Fifty-five ISS chil⁃dren were treated with recombinehuman GH [0.15 IU/(kg·d)] for threemonths to analyse the association of IGF-1 responsebook=79,ebook=84of GH treatment and genotypes.Results There were 63 GHRfl and 45 GHRd3 in 108 ISS children.There were no signifi⁃cant differences in BMI, IGF-1, IGFBP3, GH peak, IGF-1 SDS and IGFBP3 SDS between two groups (P > 0.05).Multiple stepwise regression analysis showed that age, IGFBP3, lg (BMI) and lg (GH peak) were influencing factors of lgIGF-1 (P < 0.05).In 55 ISS children treated with rhGH, there were 34 cases of GHRd3.The differences of△IGF-1 and△IGF-1 SDS werehigher in GHRd3 group than those of GHRfl group (n=21).Conclusion The GH sensitivitymay be a risk factor in ISS children, whichmay not be related with GHR polymorphism.
Key words:idiopathic short stature ; receptors, somatotropin; gene polymorphism; insulin-like growth factor 1; IGF-binding protein 3; bodymass index特发性矮小(idiopathic short stature,ISS)是指身高低于同种族、同年龄、同性别平均身高2个标准差,且排除其他特殊内分泌疾病或器质性病变的矮小症。其病因可能与生长激素(growthhormone,
通讯作者△E-mail:liugeli2001@126.com
作者简介:程炳娟(1989),女,硕士,主要从事小儿内分泌研究
中图分类号:R179
文献标志码:A
DOI:10.11958/59137
作者单位:1天津医科大学研究生院(邮编300070);2天津医科大学总医院儿科;3天津医科大学总医院核医学实验室



