李竹




【摘要】 目的:探讨N末端B型利钠肽原(NT-proBNP)水平对射血分数保留或降低的急性失代偿性心力衰竭(ADHF)患者预后的预测价值。方法:选择本院2019年1-12月收治的ADHF患者150例,记录其基本资料、用药、实验室检查、合并症、超声心动图等情况,以射血分数(EF)40%为分界值,将患者分为EF降低组(EF<40%,n=84)及EF保留组(EF≥40%,n=66);以上述每组患者NT-proBNP中位数为界值分为高NT-proBNP(NT-proBNP≥中位数)及低NT-proBNP(NT-proBNP<中位数)两个亚组,随访1年,应用COX回归模型分析NT-proBNP对EF保留或降低的ADHF患者不良事件及全因死亡的预测价值。结果:EF降低组NT-proBNP中位数为3 788 ng/L,EF保留组NT-proBNP中位数为2 850 ng/L,共有64例(42.67%)患者发生不良事件,其中全因死亡22例(14.67%)。EF降低组与EF保留组中,高NT-proBNP患者在年龄、合并心房颤动、使用利尿剂、Hb及肌酐清除率方面与低NT-proBNP患者比较,差异均有统计学意义(P<0.05)。单因素COX回归分析显示,NT-proBNP为EF保留或降低的ADHF患者不良事件发生及全因死亡的预测因素(P<0.001),校正混杂因素年龄、合并心房颤动、使用利尿剂、Hb及肌酐清除率后,多因素COX回归分析显示,高NT-proBNP为EF保留或降低的ADHF患者不良事件发生及全因死亡的独立危险因素(P<0.001),对EF保留患者的预测价值高于EF降低患者。结论:NT-proBNP为EF保留或降低的ADHF患者不良事件发生及全因死亡的独立预测因素,对EF保留患者的预测价值高于EF降低患者。
【关键词】 N末端B型利钠肽原 射血分数 急性失代偿性心力衰竭
Effect of N-terminal Pro-B-type Natriuretic Peptide Level on Prognosis of Patients with Acute Decompensated Heart Failure with Preserved or Decreased Ejection Fraction/LI Zhu. //Medical Innovation of China, 2021, 18(23): 0-056
[Abstract] Objective: To investigate the predictive value of N-terminal pro-B-type natriuretic peptide (NT-proBNP) level in the prognosis of patients with acute decompensated heart failure (ADHF) with the retention or decrease of ejection fraction. Method: A total of 150 patients in our hospital with ADHF from January 2019 to December 2019 were selected. The basic information, medication, laboratory examination, complications and echocardiography were recorded. The patients were divided into EF reduction group (EF<40%) and EF retention group (EF≥40%); patients in the two groups were divided into two subgroups according to the median NT-proBNP of each group: high NT-proBNP group (NT-proBNP≥middle value) and low NT-proBNP group (NT-proBNP<middle value). After one year follow-up, COX regression model was used to analyze the predictive value of NT-proBNP for adverse events and all-cause death in ADHF patients with preserved or reduced EF. Result: The median of
NT-proBNP in EF reduction group was 3 788 ng/L, and that of the EF retention group was 2 850 ng/L, and 64 patients (42.67%) had adverse events, of which 22 patients (14.67%) died. In the EF reduction group and EF retention group, there were significant differences in age, atrial fibrillation, diuretic use, Hb and creatinine clearance rate between high NT-proBNP patients and low NT-proBNP group (P<0.05). Single factor COX regression analysis showed that NT-proBNP was the predictor of adverse events and all-cause death in patients with EF retention or reduction (P<0.001). After correcting the confounding factors of age combined with atrial fibrillation, diuretics, Hb and creatinine clearance rate, multivariate COX regression analysis found that high NT-proBNP was an independent risk factor for adverse events and all-cause death in patients with EF retention or reduction (P<0.001), the predictive value in EF retention patients was higher than that in patients with EF reduction. Conclusion: NT-proBNP is an independent predictor of adverse events and all-cause death in patients with EF retention or reduction, the predictive value of NT-proBNP in EF retention patients is higher than that in patients with EF reduction.
[Key words] NT-proBNP Ejection fraction Acute decompensated heart failure
First-author’s address: Zhuanghe Central Hospital, Zhuanghe 116400, China
doi:10.3969/j.issn.1674-4985.2021.23.013
急性失代偿性心力衰竭(ADHF)是新发或再发的心衰症状或体征逐渐加重或急速恶化,占心力衰竭(HF)住院患者的75%,患者入院和出院的预后分析很差,高达50%的患者在6个月内再次入院或死亡[1-2]。在心力衰竭患者中,心力衰竭伴射血分数降低(EF<40%,HFrEF)的患者约占50%,2016年欧洲心脏病学会HF指南建议将EF≥40%患者进一步区分为EF中间值(HFmrEF,EF:40%~49%)和EF保留(HFpEF,EF≥50%)患者[3]。N末端B型利钠肽原(NT-proBNP)在不同射血分数的心衰患者中存在显着差异,其在ADHF住院患者中的预后价值已经得到很好的证实,尤其对HFpEF患者的研究较多[4-7],但NT-proBNP在不同EF分层患者中价值缺乏全面评估。NT-proBNP预测价值受到年龄、体重指数(BMI)、心功能分级等多种因素的影响,消除混杂因素影响从而确定NT-proBNP对不同EF分层患者预后影响至关重要,本研究就这一课题进行研究,现报道如下。
1 资料与方法
1.1 一般资料 选择本院2019年1-12月收治的ADHF患者150例。纳入标准:(1)结合症状、体征、实验室检查、超声等确诊为ADHF[8];(2)完成1年随访且临床资料完整。排除标准:(1)恶性肿瘤;(2)既往心肌梗死、心肌炎、心包疾病、肾功能不全等;(3)精神障碍;(4)急慢性感染及创伤。患者及家属知情同意本研究,且本研究经伦理委员会批准同意。
1.2 方法
1.2.1 检查、治疗及随访 患者入院后完成各项评估,询问记录症状、一般人口学信息、既往病史、家族史等,进行相应查体,抽取外周静脉血完成NT-proBNP、血钾、血钠等实验室指标检测,进行心电图、超声心动图检查。根据患者情况给予相应对因对症治疗。患者出院后进行随访,记录随访期间患者不良事件发生情况,以完成1年随访为研究终点时间,整理分析患者临床资料。
1.2.2 分组 以射血分数40%为分界值,将患者分为EF降低组(EF<40%)及EF保留组(EF≥40%);以上述每组患者NT-proBNP中位数为界值分为高NT-proBNP(NT-proBNP≥中位数)及低NT-proBNP(NT-proBNP<中位数)两个亚组,比较不同组患者的临床资料。
1.3 观察指标及评价标准 人口学信息及查体结果:性别、年龄、BMI、吸烟、饮酒、心率(HR)、舒张压、收缩压;合并症:高血压、糖尿病、心房颤动;用药情况:ACEI、ARB、MRA、β受体阻滞剂、利尿剂、地高辛、阿司匹林、他汀类药物;实验室指标:血红蛋白(Hb)、肌酐清除率、NT-proBNP;
随访1年不良事件发生情况:全因死亡及因心衰再住院;超声心动图检查结果:左室射血分数。实验室指标及左室射血分数均以入院时第一次检查结果为准。
1.4 统计学处理 所得数据采用SPSS 23.0进行统计学分析,符合正态分布的计量资料以(x±s)表示,比较用t检验;计数资料以率(%)表示,比较用χ检验;采用单变量及多变量COX回归模型分析NT-proBNP对不良事件发生的预测价值。P<0.05为差异有统计学意义。
2 结果
2.1 分组及基础资料比较 EF降低组84例,EF保留组66例;EF降低组NT-proBNP中位数为
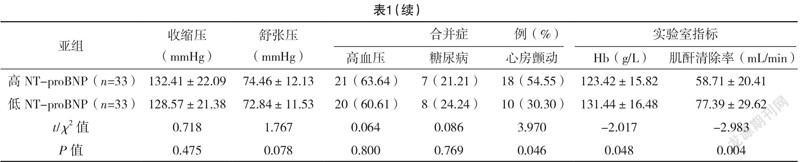
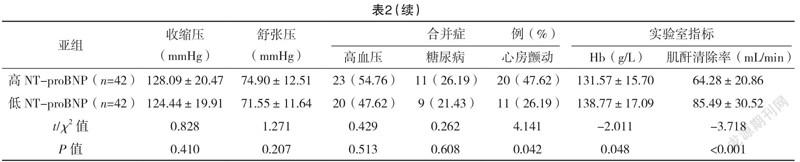
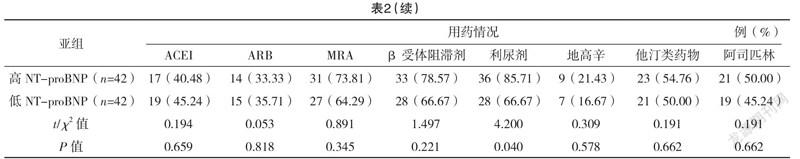
3 788 ng/L,两亚组各42例患者;EF保留组NT-proBNP中位数为2 850 ng/L,两亚组各33例患者。EF降低组与EF保留组中,高NT-proBNP患者的年龄、合并心房颤动、使用利尿剂、Hb及肌酐清除率与低NT-proBNP患者比较,差异均有统计学意义(P<0.05);两组其他指标比较,差异均无统计学意义(P>0.05)。见表1、2。
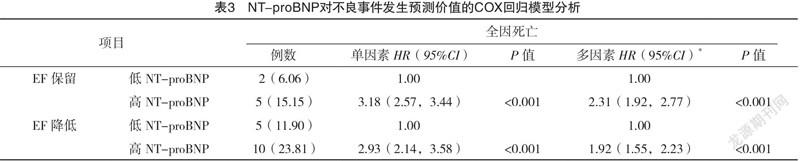
2.2 COX回归模型分析 随访1年,共有64例(42.67%)患者发生不良事件,其中全因死亡22例(14.67%)。单因素COX回归分析显示,NT-proBNP为EF保留或降低的ADHF患者不良事件发生及全因死亡的预测因素(P<0.001),校正混杂因素后,多因素COX回归分析显示,高NT-proBNP为EF保留或降低的ADHF患者不良事件发生及全因死亡的独立危险因素(P<0.001),对EF保留患者的预测价值高于EF降低患者,见表3。
3 讨论
ADHF是65岁以上老年人最常见的住院原因,其发病率、死亡率及频繁住院率均在不断增加[9-10]。在HF患者中,约一半为HFmrEF或HFpEF患者,虽然其射血分数较HFrEF患者高,但其预后并未明显改善[11]。指南推荐NT-proBNP用于HF诊断,NT-proBNP水平与心室充盈压力有关,而心室充盈压力是HFpEF、HFmrEF和HFrEF产生的关键病理生理学因素[8,11]。文献[2]荟萃分析表明,
NT-proBNP是ADHF患者不良事件及全因死亡的独立影响因子;一项纳入279名老年ADHF患者的研究表明,NT-proBNP为不良预后的独立危险因素[12];黄樱硕等[7]研究结论为NT-proBNP与HFpEF的老年ADHF患者不良预后相关。
基于以上研究,本文将ADHF患者按照EF的不同进行分层,探讨NT-proBNP在不同分层患者中的预测价值及差异,结果显示,NT-proBNP对EF保留或降低的ADHF患者不良事件发生及全因死亡均具有较高的预测价值,与Savarese等[13]针对HF患者的分层研究结果一致,但其所选患者病情较轻。Cleland等[14]研究中,NT-proBNP≥1 036.0 ng/L可以预测老年HF不良事件发生情况,而本研究中EF降低组以NT-proBNP中位数3 788 ng/L,EF保留组以NT-proBNP中位数为2 850 ng/L为界值,高NT-proBNP水平患者发生不良预后风险更高;
NT-proBNP易受性别、年龄等因素影响,此前亦有研究表明,房颤和较低的BMI与HFrEF和HFpEF中较高的NT-proBNP相关[11,15-16],本研究分析患者基础资料,EF降低组与EF保留组中,高NT-proBNP患者在年龄、合并心房颤动、使用利尿剂、Hb及肌酐清除率方面与低NT-proBNP患者比较,差异均有统计学意义(P<0.05),其他指标比较,差异均无统计学意义(P>0.05),多因素COX回归分析校正了相关混杂因素年龄、合并心房颤动、使用利尿剂、Hb及肌酐清除率的影响,提高了评估价值与准确性。
近期一项多中心研究表明,NT-proBNP在HFpEF、HFmrEF和HFrEF患者中均具有独立预测价值且在不同分层中预测价值相似[17],本研究结果中NT-proBNP对EF保留患者的预测价值高于EF降低患者,差异可能与患者选择、种族差异、病情严重程度及随访时间不同等因素有关。除了单一的NT-proBNP测量,以往研究表明NT-proBNP水平的变化也与预后相关,Savarese等[11]的研究中,55%的患者中位时间7个月后第二次测定NT-proBNP水平较之前降低,全因死亡风险降低47%,心衰住院风险降低59%;一项meta分析也表明,从基线到随访结束NT-proBNP水平的变化与心衰住院风险的降低有关[18]。
本研究局限性及不足之处:(1)由于病例数较少,未对HFmrEF患者进行单独研究,NT-proBNP水平对单纯HFmrEF患者的影响未知;(2)NT-proBNP存在动态变化,本研究仅对入院时基线NT-proBNP水平进行研究,未就其出院时水平及动态变化对预后的影响进行研究。
综上所述,NT-proBNP为EF保留或降低的ADHF患者不良事件发生及全因死亡的独立预测因素,对EF保留患者的预测价值高于EF降低患者;NT-proBNP水平对单纯HFmrEF患者预后影响及其动态变化对不同EF的ADHF患者影响仍需进一步扩大样本量进行长期临床研究。
参考文献
[1] Stienen S,Salah K,Moons A H,et al.NT-proBNP (N-Terminal pro-B-Type Natriuretic Peptide)-Guided Therapy in Acute Decompensated Heart Failure: PRIMA Ⅱ Randomized Controlled Trial (Can NT-ProBNP-Guided Therapy During Hospital Admission for Acute Decompensated Heart Failure Reduce Mortality and Readmissions?)[J].Circulation,2018,137(16):1671-1683.
[2] Santaguida P L,Don-Wauchope A C,Oremus M,et al.BNP and NT-proBNP as prognostic markers in persons with acute decompensated heart failure: a systematic review[J].Heart Fail Rev,2014,19(4):453-470.
[3] Ponikowski P,Voors A A,Anker S D,et al.2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC[J].Eur Heart J,2016,37(27):2129-2200.
[4] Salah K,Stienen S,Pinto Y M,et al.Prognosis and NT-proBNP in heart failure patients with preserved versus reduced ejection fraction[J].Heart,2019,105(15):1182-1189.
[5] Kang S H,Park J J,Choi D J,et al.Prognostic value of NT-proBNP in heart failure with preserved versus reduced EF[J].Heart,2015,101:1881-1888.
[6]曹娟,金雪娟,周俊,等.N末端B型利钠肽原对射血分数保留的心力衰竭患者全因死亡的预测价值[J].中华心血管病杂志,2019,47(11):875-881.
[7]黄樱硕,王倩倩,孙颖,等.老年急性失代偿射血分数保留的心力衰竭患者N末端B型利钠肽水平及变化与预后关系[J].中华老年医学杂志,2018,37(1):4-8.
[8]中华医学会心血管病学分会心力衰竭学组,中国医师协会心力衰竭专业委员会中华心血管病杂志编辑委员会.中国心力衰竭诊断和治疗指南2018[J].中华心血管病杂志,2018,46(10):760-789
[9] Abdo A S.Hospital Management of Acute Decompensated Heart Failure[J].Am J Med Sci,2017,353(3):265-274.
[10] Teerlink J R, Alburikan K,Metra M,et al.Acute decompensated heart failure update[J].Curr Cardiol Rev,2015,11(1):53-62.
[11] Savarese G,Hage C,Orsini N,et al.Reductions in N-Terminal Pro-Brain Natriuretic Peptide Levels Are Associated with Lower Mortality and Heart Failure Hospitalization Rates in Patients with Heart Failure with Mid-Range and Preserved Ejection Fraction[J/OL].
Circ Heart Fail,2016,9(11):e003105.
[12] Passantino A,Guida P,Lagioia R,et al.Predictors of Long-Term Mortality in Older Patients Hospitalized for Acutely Decompensated Heart Failure: Clinical Relevance of Natriuretic Peptides[J].J Am Geriatr Soc,2017,65(4):822-826.
[13] Savarese G,Orsini N,Hage C,et al.Associations with and Prognostic and Discriminatory Role of N-Terminal Pro-B-Type Natriuretic Peptide in Heart Failure with Preserved Versus Mid-range Versus Reduced Ejection Fraction[J].J Card Fail,2018,24(6):365-374.
[14] Cleland J G,Taylor J,Freemantle N,et al.Relationship between plasma concentrations of N-terminal pro brain natriuretic peptide and the characteristics and outcome of patients with a clinical diagnosis of diastolic heart failure: a report from the PEP-CHF study[J].Eur J Heart Fail,2012,14(5):487-494.
[15] Lam C S,Rienstra M,Tay W T,et al.Atrial Fibrillation in Heart Failure With Preserved Ejection Fraction: Association With Exercise Capacity, Left Ventricular Filling Pressures, Natriuretic Peptides, and Left Atrial Volume[J].JACC Heart Fail,2017,5(2):92-98.
[16] Francis G S,Felker G M,Tang W H.A Test in Context: Critical Evaluation of Natriuretic Peptide Testing in Heart Failure[J].J Am Coll Cardiol,2016,67(3):330-337.
[17] Lam C S P,Gamble G D,Ling L H,et al.Mortality associated with heart failure with preserved vs. reduced ejection fraction in a prospective international multi-ethnic cohort study[J].Eur Heart J,2018,39:1770-1780.
[18] Savarese G,Musella F,D’Amore C,et al.Changes of natriuretic peptides predict hospital admissions in patients with chronic heart failure: a meta-analysis[J].JACC:Heart Failure,2014,2(2):148-158.
(收稿日期:2021-07-07) (本文编辑:张爽)



