张宝山 张海军 陈会校 赵沙沙 张强 李娟 柴巧英

摘要:目的 探讨经皮冠状动脉介入(PCI)术后72 h内血压变异性(BPV)对ST段抬高型心肌梗死(STEMI)患者随访主要心血管不良事件(MACE)发生风险的影响,旨在为后续个体化防治方案制定及预后评估提供更多证据。方法 回顾性纳入2017年1月-2020年6月于邯钢医院行直接PCI术治疗的STEMI患者共359例,根据术后72 h内收缩压和舒张压变异性分为高水平组和低水平组,比较各组临床特征资料及随访24个月MACE发生情况。采用Logistic回归模型评价PCI术后72 h内动态BPV对STEMI患者术后随访24个月MACE发生风险的独立影响,描绘ROC曲线评价PCI术后72 h内动态BPV用于随访MACE发生风险预测临床效能。结果 收缩压变异性高水平组房颤比例、高血压比例及ACEI/ARB使用比例均高于低水平组(P<0.05);舒张压变异性高水平组高血压比例、体质量指数及ACEI/ARB使用比例均高于低水平组,但年龄和LVEF水平均低于低水平组(P<0.05);收缩压变异性高水平组心力衰竭发生率高于低水平组(P<0.05);舒张压变异性高水平组心力衰竭和MACE发生率均高于低水平组(P<0.05);Logistic回归模型多因素分析结果显示,整体人群中收缩压高变异性是心力衰竭发生独立危险因素,舒张压高变异性是心力衰竭及MACE发生独立危险因素(P<0.05);而口服降压药物人群中收缩压和舒张压高变异性均是心力衰竭及MACE发生独立危险因素(P<0.05)。ROC曲线分析结果显示,舒张压高变异性可用于STEMI患者PCI术后随访24个月MACE发生风险预测,AUC=0.863(95%CI:0.783~0.923)。结论 STEMI患者随访MACE发生与PCI术后72 h内动态BPV水平关系密切,且收缩压和舒张压变异性联合在预测患者术后24个月MACE发生风险方面效能良好。
关键词:经皮冠状动脉介入;血压变异性;ST段抬高型心肌梗死;主要心血管不良事件
中图分类号:R541.4 文献标识码:A DOI:10.3969/j.issn.1006-1959.2024.12.017
文章编号:1006-1959(2024)12-0080-05
Influence of BPV Within 72-hour After PCI on MACE Risk During Follow-up in Patients with STEMI
Abstract:Objective To investigate the effect of blood pressure variability (BPV) within 72-hour after percutaneous coronary intervention (PCI) on the risk of major adverse cardiovascular events (MACE) in patients with ST-segment elevation myocardial infarction (STEMI) during follow-up, so as to provide more evidence for subsequent individualized prevention and prognosis evaluation.Methods A total of 359 STEMI patients who underwent primary PCI in Hangang Hospital from January 2017 to June 2020 were retrospectively included. According to the variability of systolic and diastolic blood pressure within 72-hour after operation, they were divided into high-level group and low-level group. The clinical characteristics of each group and the occurrence of MACE after 24 months of follow-up were compared. Logistic regression model was used to evaluate the independent effect of dynamic BPV within 72-hour after PCI on the risk of MACE in STEMI patients after 24 months of follow-up. The ROC curve was used to evaluate the clinical efficacy of dynamic BPV within 72-hour after PCI in predicting the risk of MACE.Results The proportion of atrial fibrillation, hypertension and ACEI/ ARB used in high-level group of systolic blood pressure variability were higher than those in low-level group (P<0.05). The proportion of hypertension, body mass index and proportion of ACEI/ARB used in high-level group of diastolic blood pressure variability were higher than those in low-level group, but the age and LVEF levels were lower than those in the low-level group (P<0.05). The incidence of heart failure in high-level group of systolic blood pressure variability was higher than that in low-level group (P<0.05). The incidence of heart failure and MACE in high-level group of diastolic blood pressure variability was higher than that in low-level group(P<0.05). Multivariate analysis of Logistic regression model showed that high variability of systolic blood pressure was an independent risk factor for heart failure in the whole population, and high variability of diastolic blood pressure was an independent risk factor for heart failure and MACE (P<0.05); while, the high variability of systolic blood pressure and diastolic blood pressure in the population of oral antihypertensive drugs is an independent risk factor for heart failure and MACE (P<0.05). ROC curve analysis showed that high diastolic blood pressure variability could be used to predict the risk of MACE in STEMI patients after PCI for 24 months, AUC=0.863(95%CI: 0.783-0.923).Conclusion The occurrence of MACE in STEMI patients during follow-up is closely related to the dynamic BPV level within 72-hour after PCI, and the combination of systolic blood pressure and diastolic blood pressure variability is effective in predicting the risk of MACE 24 months after PCI.
Key words:Percutaneous coronary intervention;Blood pressure variability;ST-segment elevation myocardial infarction;Major cardiovascular adverse events
近年来研究提示,BPV水平与冠状动脉粥样硬化性心脏病、急性心肌梗死、心力衰竭及卒中发生关系密切,其中收缩压变异性可用于心血管疾病发生率及继发死亡风险预测[1-3]。有学者报道证实,STEMI患者接受PCI术后住院期间收缩压变异性与临床预后独立相关;同时BVP还是急性心肌梗死患者住院及术后12个月MACE发生风险独立预测因子[4,5]。但对于术后短期,即0~3 d内BVP水平与行PCI术治疗STEMI患者心血管预后及死亡风险间关系报道相对较少,缺乏充足循证医学证据。基于此,本研究通过回顾性分析2017年1月-2020年6月于邯钢医院行直接PCI术治疗STEMI患者共359例临床特征资料,以及随访24个月MACE发生情况,评估PCI术后72 h内动态BPV对STEMI患者随访MACE发生风险的影响,旨在为后续个体化防治方案制定及预后评估提供更多证据。
1资料与方法
1.1一般资料 回顾性纳入2017年1月-2020年6月于邯钢医院行直接PCI术治疗STEMI患者共359例,根据术后72 h内收缩压和舒张压变异性分为高水平组和低水平组,其中≥中位值为高水平组,<中位值为低水平组。研究设计符合世界医学大会《赫尔辛基宣言》要求,研究方案经医院伦理委员会批准,研究对象知情同意,并签署同意书。
1.2纳入与排除标准 纳入标准:①符合STEMI诊断标准,其中新发或疑似新发左束支传导阻滞合并心肌肌钙蛋白I水平升高亦归入其中[6];②接受直接PCI术且完成药物洗脱支架植入;③年龄18~75岁;④随访24个月及以上。排除标准:①术后30 d内死亡;②活动性炎症;③自身免疫性疾病;④恶性肿瘤。
1.3资料收集 登录医院电子病历系统收集患者性别、年龄、既往史、超声心动图、实验室检查及药物治疗情况等资料,其中吸烟指既往连续或累计吸烟≥6个月[7];血脂异常判定标准为LDL-C≥3.4 mmol/L、HDL-C<1.04 mmol/L、TG≥1.7 mmol/L或正在接受降脂治疗[8]。术后0.5 h起持续至72 h的动态血压监测(迈瑞MC6800型动态血压监测仪)每隔1 h记录1次血压,计算个体内血压值标准差,收缩压和舒张压标准差中位数分别为12.1 mmHg,8.9 mmHg。
1.4随访情况 术后随访采用电话、门诊或住院复查方式完成,每3~6个月随访1次;记录术后24个月内MACE发生情况,包括心力衰竭、因胸痛症状再次入院、靶血管重建及心源性死亡;其中靶血管重建指PCI术后24个月再行冠状动脉造影证实狭窄程度≥70%而再次接受血运重建手术治疗[9]。
1.5统计学处理 数据分析采用SPSS 20.0软件。采用Kolmogorov-Smirnov检验完成正态性评估,符合正态分布计量资料比较采用t检验,以(x±s)表示;计数资料比较采用χ2检验,以(%)表示;多因素分析采用Logistic回归模型,描绘ROC曲线评价预测效能。P<0.05为差异有统计学意义。
2结果
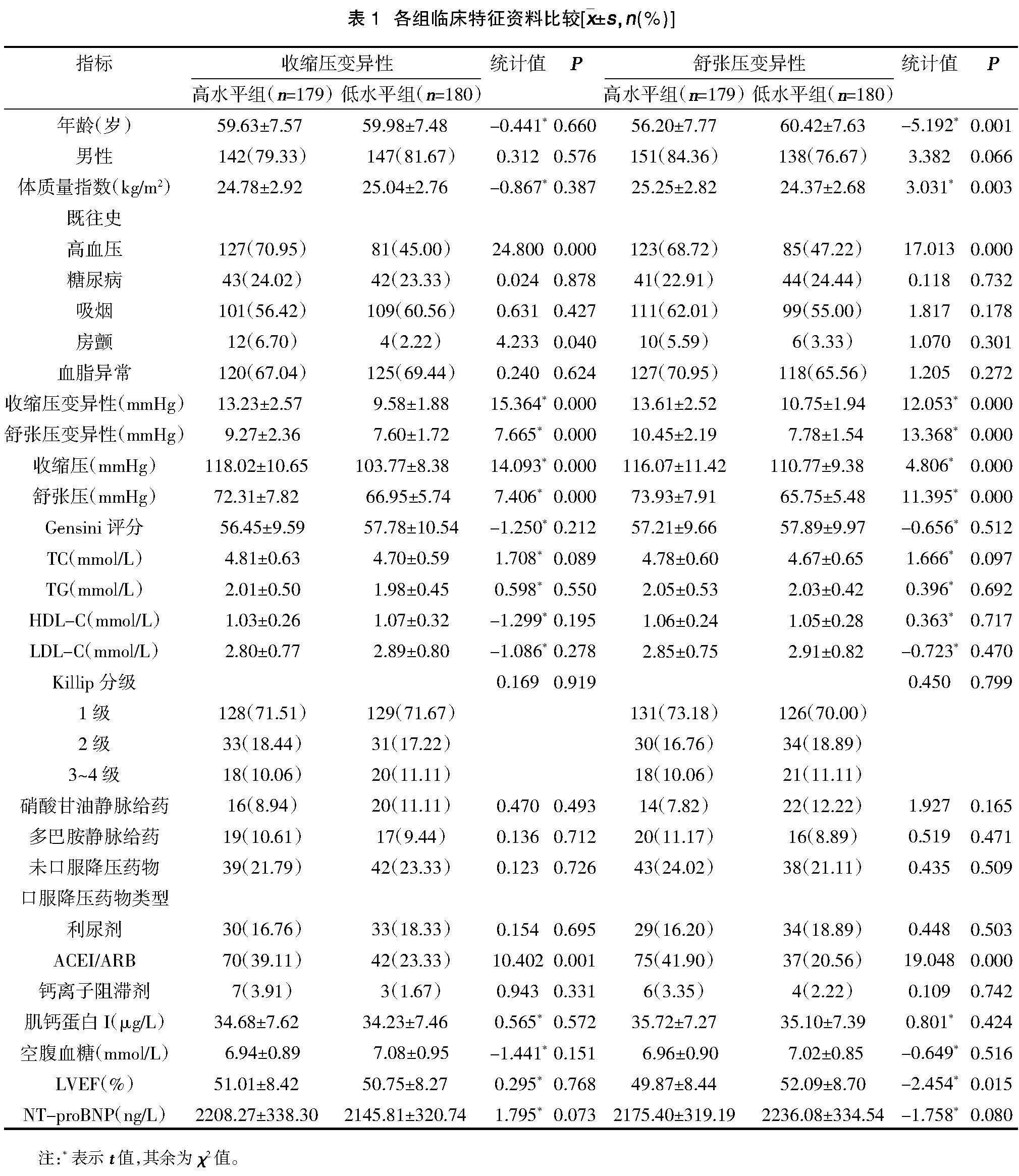
2.1各组临床特征资料比较 收缩压变异性高水平组房颤比例、高血压比例及ACEI/ARB使用比例均高于低水平组(P<0.05);舒张压变异性高水平组高血压比例、体质量指数及ACEI/ARB使用比例均高于低水平组(P<0.05),但年龄和LVEF水平均低于低水平组(P<0.05),见表1。
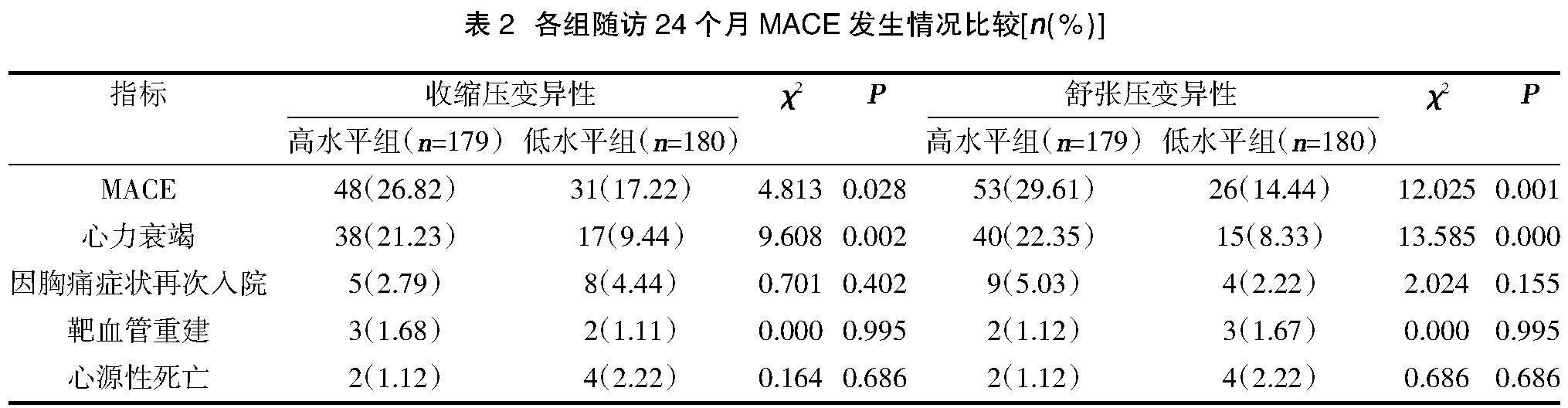
2.2各组随访24个月MACE发生情况比较 收缩压变异性高水平组心力衰竭发生率高于低水平组(P<0.05);舒张压变异性高水平组心力衰竭和MACE发生率均高于低水平组(P<0.05),见表2。
2.3 PCI术后72 h内动态BPV对STEMI患者术后随访24个月MACE发生风险的影响多因素分析 Logistic回归模型多因素分析结果显示,整体人群中收缩压高变异性是心力衰竭发生独立危险因素(P<0.05);舒张压高变异性是心力衰竭及MACE发生独立危险因素(P<0.05);而口服降压药物人群中收缩压和舒张压高变异性均是心力衰竭及MACE发生独立危险因素(P<0.05),见表3。
2.4 PCI术后72 h内动态BPV用于术后随访24个月MACE发生风险预测临床效能ROC曲线分析 ROC曲线分析结果显示,舒张压高变异性可用于STEMI患者PCI术后随访24个月MACE发生风险预测,AUC=0.863(95%CI:0.783~0.923),见图1。
3讨论
血压波动与人体体液、神经中枢反射及周围环境等相互影响关系密切。在单日或就诊期间测量血压变化情况可能与疾病本身、药物相关损伤或血流动力学调节系统异常有关,并能够在一定程度上反映机体整体健康状况[10,11]。
既往研究亦证实,BPV水平与卒中、心肌梗死、心血管病发生发展有关,并能够用于心血管疾病患者全因死亡预测,而上述事件与患者平均血压水平并无相关性[12]。动态血压监测是评估24 h内BPV最常用手段之一,经动态血压监测每隔1 h计算BPV是全人群心血管意外相关死亡风险独立预测因子;同时血压正常急性冠脉综合征患者经动态血压监测评估短期 BPV高水平与PCI后再狭窄风险独立相关[13,14]。此外,基于动态血压监测计算BPV还可能与急性心肌梗死患者住院期间MACE发生风险有关[15]。
本研究通过单因素和多因素分析,证实术后早期BPV这一指标与STEMI患者直接PCI术后MACE发生风险具有相关性;其中整体人群中收缩压高变异性是患者心力衰竭发生独立危险因素,而舒张压高变异性则与心力衰竭及MACE发生独立相关,与以往报道结果基本相符。进一步针对接受口服降压药治疗人群进行亚组分析结果显示,收缩压和舒张压高变异性均是心力衰竭及MACE发生独立危险因素,提示即使接受口服降压药物治疗甚至将平均血压控制在合理水平,仍应关注BPV对于远期预后的影响。此外本次研究还发现,收缩压变异性较低人群具有更高心源性死亡率,这是以往报道中未观察到的现象,但具体原因尚不明确,考虑到研究整体样本量较小,这一现象仍有待后续更大规模前瞻性研究确证。有报道提示[16,17],急性心肌梗死后心力衰竭患者低BPV与低脉压有关,而低脉压往往提示每搏输出量低,故与远期不良预后有关。另有研究提示[18-20],BPV水平增加可能与大动脉僵硬及顺应性下降有关;同时交感神经活动异常增强可导致血压不稳定,而这往往与伴心血管不良事件发生风险增加直接相关;此外部分体外实验结果提示,高BPV水平能够导致或加重内皮损伤,刺激肾素血管紧张素系统及心肌细胞凋亡,最终反映为终末脏器功能持续受损。以上皆可能是高BPV水平与急性心肌梗死患者预后不良相关潜在原因。
综上所述,STEMI患者随访MACE发生与PCI术后72 h内动态BPV水平关系密切,且收缩压和舒张压变异性联合在预测患者术后24个月MACE发生风险方面效能良好。但研究仍存在不足:①属于单中心回顾性研究,导致选择偏倚无法避免;②因无法准确记录降压药物用量及患者情绪状态,所得结论仍有待后续更为严谨前瞻性研究确证。
参考文献:
[1]Rodríguez-Jiménez AE,Negrín-Valdés T,Cruz-Inerarity H,et al.Prognostic Scale to Stratify Risk of Intrahospital Death in Patients with Acute Myocardial Infarction with ST-Segment Elevation [J].MEDICC Rev,2020,22(3):46-53.
[2]Messerli FH,Hofstetter L,Rimoldi SF,et al.Risk factor varia bility and cardiovascular outcome:JACC review topic of the week [J].J Am Coll Cardiol,2019,73(20):2596-2603.
[3]Mahfouz RA,El-Shetry M,Frere A,et al.Blood Pressure Variability and Atrial Fibrillation in Patients with Acute ST Segment Elevation Myocardial Infarction: The Relation with Left Atrial Electromechanical Delay - A 1-Year Follow-Up Study [J].Pulse(Basel),2020,8(1-2):57-65.
[4]Kang J,Kim BJ,Yang MH,et al.Blood pressure variability in subacute stage and risk of major vascular events in ischemic stroke survivors[J].J Hypertens,2019,37(10):2000-2006.
[5]Soh MS,Park JS,Seo KW,et al.Visit-to-visit systolic blood pressure variability in patients with ST-elevation myocardial infarction predicts long-term cardiovascular outcomes[J].J Hum Hypertens,2019,33(4):259-266.
[6]中华医学会心血管病学分会,中华心血管病杂志编辑委员会.急性ST段抬高型心肌梗死诊断和治疗指南[J].中华心血管病杂志,2015,43(5):380-393.
[7]Shao C,Wang J,Li P,et al.Evaluation of a risk index for predicting short-term and long-term outcomes in patients with ST-elevation myocardial infarction [J].Catheter Cardiovasc Interv,2020,95(Suppl 1):542-549.
[8]Mouhat B,Putot A,Hanon O,et al.Low Systolic Blood Pressure and Mortality in Elderly Patients After Acute Myocardial Infarction [J].J Am Heart Assoc,2020,9(5):e013030.
[9]Simsek Z,Zehir R,Kalkan S,et al.Inter-arm blood pressure difference is associated with contrast-induced nephropathy in patients with ST-segment elevation myocardial infarction who underwent primary percutaneous coronary intervention [J].Clin Exp Hypertens,2022,44(3):258-262.
[10]Konstantinou K,Tsioufis C,Mantzouranis E,et al.Blood pressure variability as a predictor of cardiovascular outcomes in patients with acute myocardial infarction[J].J Hypertens,2019,37:e301.
[11]Song MS,Choi YJ,Kim H,et al.Relationship between blood pressure levels and ischemic stroke, myocardial infarction, and mortality in very elderly patients taking antihypertensives:a nationwide population-based cohort study[J].BMC Geriatr,2021,21(1):620-627.
[12]Tang Y,Liu S,Shi Y,et al.Association of blood pressure in the first-week of hospitalization and long-term mortality in patients with acute left ventricular myocardial infarction [J].Int J Cardiol,2022,349(2):18-26.
[13]Maznyczka AM,McCartney PJ,Oldroyd KG,et al.Risk Stratification Guided by the Index of Microcirculatory Resistance and Left Ventricular End-Diastolic Pressure in Acute Myocardial Infarction[J].Circ Cardiovasc Interv,2021,14(2):e009529.
[14]Pamukcu HE,A?ikel S.Prognostic Value of Elevated Pulmonary Artery Systolic Pressure on Short Term in Patients With Acute Myocardial Infarction[J].Angiology,2020,71(10):967-974.
[15]Rambod M,Rakhshan M,Tohidinik S,et al.The effect of lemon inhalation aromatherapy on blood pressure, electrocardiogram changes, and anxiety in acute myocardial infarction patients: A clinical, multi-centered, assessor-blinded trial design [J].Complement Ther Clin Pract,2020,39(5):101155.
[16]Konstantinou K,Tsioufis C,Mantzouranis E,et al.Blood pressure variability as a predictor of heart failure events in patients with myocardial infarction[J].J Hypertens,2019,37:e78.
[17]Hsu PC,Lee WH,Chiu CA,et al.Usefulness of ankle-brachial index calculated using diastolic blood pressure for prediction of mortality in patients with acute myocardial infarction [J].J Clin Hypertens (Greenwich),2020,22(11):2044-2050.
[18]Pei J,Wang X,Xing Z,et al.Association between admission systolic blood pressure and major adverse cardiovascular events in patients with acute myocardial infarction [J].PLoS One,2020,15(6):e0234935.
[19]Smith TO,Sillito JA,Goh CH,et al.Association between different methods of assessing blood pressure variability and incident cardiovascular disease, cardiovascular mortality and all-cause mortality: a systematic review[J].Age Ageing,2020,49(2):184-192.
[20]Song PS,Lee SH,Jeon KH,et al.Blood Pressure at 6 Months After Acute Myocardial Infarction and Outcomes at 2 Years: The Perils Associated With Excessively Low Blood Pressures[J].Can J Cardiol,2020,36(10):1641-1648.



