邹正渝 胡龙娇 许洲松 于倩 赵常亮

【摘 要】目的 探讨桔梗成分木犀草素与磺胺嘧啶银联合治疗浅Ⅱ度烫伤的协同作用,为优化治疗方案提供新的理论基础。方法 构建SD大鼠浅Ⅱ度烫伤模型,依据给药情况分为五组:A组为模型组,B组为磺胺嘧啶银组,C组为木犀草素组,D组为磺胺嘧啶银和木犀草素联用组,N组为正常对照组。根据给药第4天和第7天的创面愈合率评价不同给药组的疗效。通过测量大鼠烫伤区域伤口直径,采用苏木精-伊红(HE)染色观察创面皮肤组织的病理变化,采用Western blot检测大鼠创面皮肤组织血管内皮生长因子(VEGF)、基质金属蛋白酶2(MMP-2)和Ⅰ型胶原蛋白(Coll-Ⅰ)表达,采用ELISA检测大鼠的肿瘤坏死因子α(TNF-α)、白细胞介素10(IL-10)水平。结果 B组、C组第7天烫伤创面愈合率均高于A组(P<0.05);D组第7天烫伤创面愈合率均高于A组、B组、C组(P<0.05)。D组皮肤层完整,角质层、表皮和真皮结构正常,皮肤毛囊及附属结构基本完整,恢复程度优于B组和C组。B组、C组VEGF、Coll-Ⅰ水平高于A组,MMP-2水平低于A组(P<0.05);B组和C组VEGF、Coll-Ⅰ、MMP-2水平比较,差异无统计学意义(P>0.05);D组VEGF、Coll-Ⅰ水平均高于A组、B组、C组,MMP-2水平均低于A组、B组、C组(P<0.05)。B组、C组TNF-α水平均低于A组(P<0.05);B组、C组TNF-α水平比较,差异无统计学意义(P>0.05);A组、B组、C组IL-10水平比较,差异无统计学意义(P>0.05);D组TNF-α水平均低于A组、B组、C组,IL-10水平均高于A组、B组、C组(P<0.05)。结论 磺胺嘧啶银联合木犀草素治疗浅Ⅱ度烫伤的效果优于单独用药,其潜在机制之一可能是通过下调MMP-2表达,上调VEGF、Coll-Ⅰ和IL-10表达,抑制TNF-α等因子的表达,以减轻组织炎症,改善烫伤创面皮肤组织环境,促进愈合。
【关键词】木犀草素;磺胺嘧啶银;浅Ⅱ度烫伤;创面愈合
中图分类号:R285 文献标识码:A 文章编号:1004-4949(2023)24-0114-05
基金项目:九龙坡区科技计划项目(编号:2021-02-011-Y)
Study on the Effect of Luteolin Extracted from Platycodon Grandiflorum Combined with Silver Sulfadiazine in the Treatment of Superficial Degree Ⅱ Scalds
ZOU Zheng-yu1,2, HU Long-jiao3, XU Zhou-song1, YU Qian4, ZHAO Chang-liang5
(1.Medical Laboratory of Chongqing Jiulongpo Peoples Hospital, Chongqing 400050, China; 2.Jiulongpo District Yangjiaping Street Community Health Service Center, Chongqing 400050, China; 3.Pharmacy department of Chongqing Jiulongpo Peoples Hospital, Chongqing 400050, China;4.Institute of Life Sciences, Chongqing Medical University, Chongqing 400021, China;5.Rehabilitation Medicine Department of Chongqing Jiulongpo Peoples Hospital, Chongqing 400050, China)
【Abstract】Objective To investigate the synergistic effect of luteolin extracted from platycodon grandiflorum and silver sulfadiazine in the treatment of superficial degree Ⅱ scalds, providing new theoretical basis for optimizing the treatment plan. Methods SD rat model of superficial degree Ⅱ scald was constructed and divided into five groups according to the administration : group A was the model group, group B was the sulfadiazine silver group, group C was the luteolin group, group D was the sulfadiazine silver and luteolin combination group, and group N was the normal control group. The efficacy of different administration groups was evaluated according to the wound healing rate on the 4th and 7th day of administration. The wound diameter in the scalded area of rats was measured. The pathological changes of wound skin tissue were observed by hematoxylineosin (HE) staining. The expressions of vascular endothelial growth factor (VEGF), matrix metalloproteinase 2 (MMP-2) and type I collagen (Coll-Ⅰ) in wound skin tissue of rats were detected by Western blot. The levels of tumor necrosis factor-α (TNF-α) and interleukin-10 (IL-10) in rats were detected by ELISA. Results The healing rate of scald wounds in group B and group C was higher than that in group A on the 7th day (P<0.05). The healing rate of scald wounds in group D was higher than that in group A, group B and group C on the 7th day (P<0.05). The skin layer of group D was intact, the structure of stratum corneum, epidermis and dermis was normal, and the skin hair follicles and accessory structures were basically intact, the degree of recovery was better than that of group B and group C. The levels of VEGF and Coll-Ⅰ in group B and group C were higher than those in group A, and the level of MMP-2 was lower than that in group A (P<0.05). There was no significant difference in the levels of VEGF, Coll-Ⅰ and MMP-2 between group B and group C (P>0.05). The levels of VEGF and Coll-Ⅰ in group D were higher than those in group A, group B and group C, and the levels of MMP-2 were lower than those in group A, group B and group C (P<0.05). The levels of TNF-αin group B and group C were lower than those in group A (P<0.05). There was no significant difference in the level of TNF-αbetween group B and group C (P>0.05). There was no significant difference in IL-10 level among group A, group B and group C (P>0.05). The level of TNF-α in group D was lower than that in group A, group B and group C, and the level of IL-10 was higher than that in group A, group B and group C (P<0.05). Conclusion The effect of silver sulfadiazine combined with luteolin in the treatment of superficial degree Ⅱ scalds is better than that of single drug. One of the potential mechanisms may be to down-regulate the expression of MMP-2, up-regulate the expression of VEGF, Coll-I and IL-10, and inhibit the expression of TNF-α and other factors, so as to reduce tissue inflammation, improve the skin tissue environment of scald wounds and promote healing.
【Key words】Luteolin; Sliver sulfadiazine; Superficial degree Ⅱ scald; Wound healing
桔梗是桔梗科植物桔梗的干燥根,含有皂苷、黄酮类、甾醇类、脂肪酸等多种化合物,具有镇咳、抗炎、降血糖、降血压等作用[1]。木犀草素(luteolin)广泛存在于桔梗等药用植物中,具有抗氧化、抗炎、抗菌等生物活性,常被用来制作药物以预防和治疗疾病[2]。磺胺嘧啶银(sliver sulfadiazine)属于磺胺类抗菌药物,是临床烧烫伤的常用外用药物之一[3]。有研究发现[4],桔梗提取物木犀草素是桔梗促进皮肤烫伤大鼠创面愈合的有效成分,可减少炎症因子释放,促进血管生成。本研究旨在通过联合使用木犀草素和磺胺嘧啶银干预大鼠浅Ⅱ度烫伤模型的愈合过程,以期寻找一种更为有效的烫伤综合治疗方案,现报道如下。
1 材料与方法
1.1 实验动物和药品 选取20只成年雄性清洁级SD大鼠,体重220~250 g,由湖南斯莱克景达实验动物有限公司提供[许可证号:SCXK(湘)2019-0004]。大鼠饲养和建模过程在重庆威斯腾生物医药科技有限责任公司进行,分笼饲养,室内温度23 ℃~25 ℃,自由饮水进食,动物进入动物房适应性饲养1周后进入实验。木犀草素购自北京索莱宝科技有限公司,磺胺嘧啶银购自美国MedChemExpress公司。
1.2 试剂 多聚甲醛和水合氯醛购自生工生物工程(上海)股份有限公司;脱毛膏购自广州露韩秀生物技术有限公司;苏木素-伊红染液(hematoxylin-eosin,HE)购自碧云天;中性树脂购自国药集团;肿瘤坏死因子α(tumor necrosis factor-α,TNF-α)和白细胞介素10(interleukin-10,IL-10)ELISA试剂盒购自达科为;血管内皮生长因子(vascular endothelial growth factor,VEGF)兔抗体购自HUABIO公司;基质金属蛋白酶-2(matrix metallopeptidase-2,MMP-2)兔抗体和Ⅰ型胶原蛋白(collagen type Ⅰ,Coll-Ⅰ)兔抗体购自美国Affinity公司;GAPDH兔抗体购自华安公司;HRP标记山羊抗兔IgG购自碧云天。
1.3 建模方法 建模前12 h禁食,腹腔注射7%水合氯醛(5 ml/kg),待充分麻醉后,使用脱毛膏脱去背部待烫伤区域被毛,将直径15 mm、重量0.5 kg的金属板块置于水浴锅中加热至65 ℃,将其均匀地放在大鼠背部脱毛区域3 s,造成约10%的烫伤创面以构建浅Ⅱ度烫伤模型。大鼠背部两侧均进行建模。
1.4 给药方法 根据给药处理将烫伤大鼠模型分为五组:A组为模型组,B组为磺胺嘧啶银组,C组为木犀草素组,D组为磺胺嘧啶银和木犀草素联用组,N组为正常对照组,每组3只大鼠,另5只大鼠备用。每天上午9点和下午3点给药。在给药之前,用生理盐水清洗伤口以去除残余物质,然后将相应的软膏按照说明书要求涂抹在伤口上,厚度约为1.5 mm[3],D组每次先涂抹磺胺嘧啶银待药物充分吸收后再涂抹木犀草素,A组不做任何给药,N组不予任何处理。
1.5 观察指标
1.5.1创面愈合率 分别在给药后第4天和第7天测量烫伤创面区域的直径,计算创面面积和创面愈合率。创面愈合率=(原始创面面积-观察创面面积)/原始创面面积×100%。创面面积越小说明创面愈合越快。
1.5.2组织检测 在给药后第8天,取两侧烫伤区域的皮肤,一侧皮肤使用4%多聚甲醛固定,4 ℃冰箱保存,用于HE染色,另一侧皮肤于-80 ℃冰箱保存,用于蛋白质印迹法(Western blot,WB)检测。HE染色评估烫伤区域表皮组织,WB检测烫伤创面皮肤组织的MMP-2、Coll-Ⅰ和VEGF的表达。
1.5.3血清检测 在给药后第8天,进行腹主动脉采血,收集血清,置于-20 ℃冰箱保存,采用ELISA方法检测TNF-α、IL-10水平。
1.6 统计学方法 使用SPSS 20.0统计学软件分析本研究数据,正态分布的计量资料以(x-±s)表示,进行方差分析,两组组间比较采用SNK法;非正态分布的计量资料以[M(P25,P75)]表示,组间比较采用Mann-Whitney U检验;以P<0.05表示差异有统计学意义。
2 结果
2.1 五组烫伤创面愈合率比较 四组第4天烫伤创面愈合率比较,差异无统计学意义(P>0.05);B组、C组第7天烫伤创愈合率均高于A组(P<0.05);D组第7天烫伤创面愈合率均高于A组、B组、C组(P<0.05),见表1。

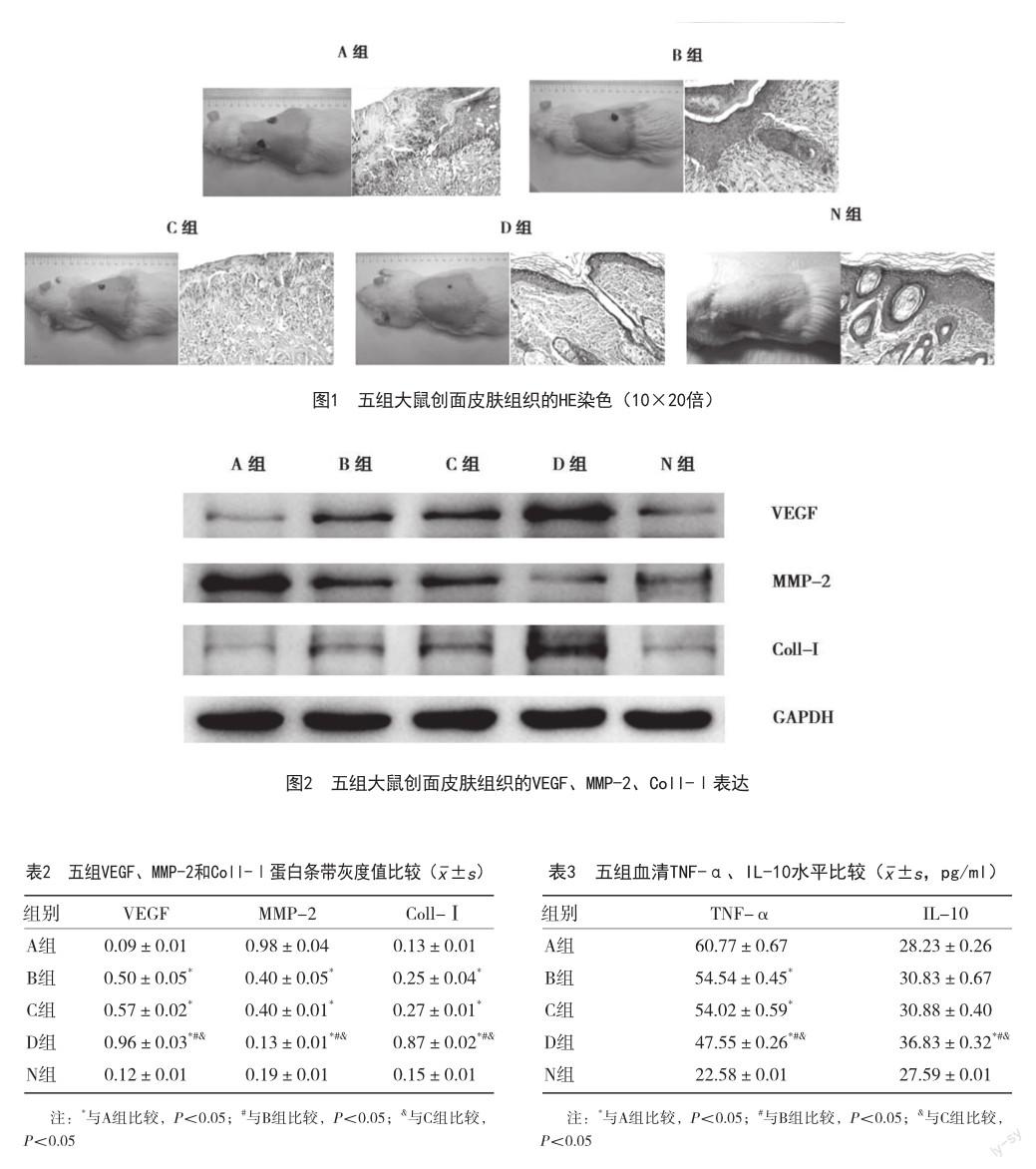
2.2 五组创面皮肤组织的病理变化 A组表皮结构破坏,组织水肿坏死,炎性细胞增多;B组、C组表皮修复良好,其中B组部分上皮再生修复,有散在炎性渗出,上皮下有瘢痕增生;C组上皮部分缺失,瘢痕样增生明显,表面有部分炎性渗出;D组皮肤层完整,角质层、表皮和真皮结构正常,皮肤毛囊及附属结构基本完整,恢复程度优于B组和C组;N组皮肤表皮完整,角质层、表皮和真皮结构正常,皮肤毛囊及附属结构完整,见图1。
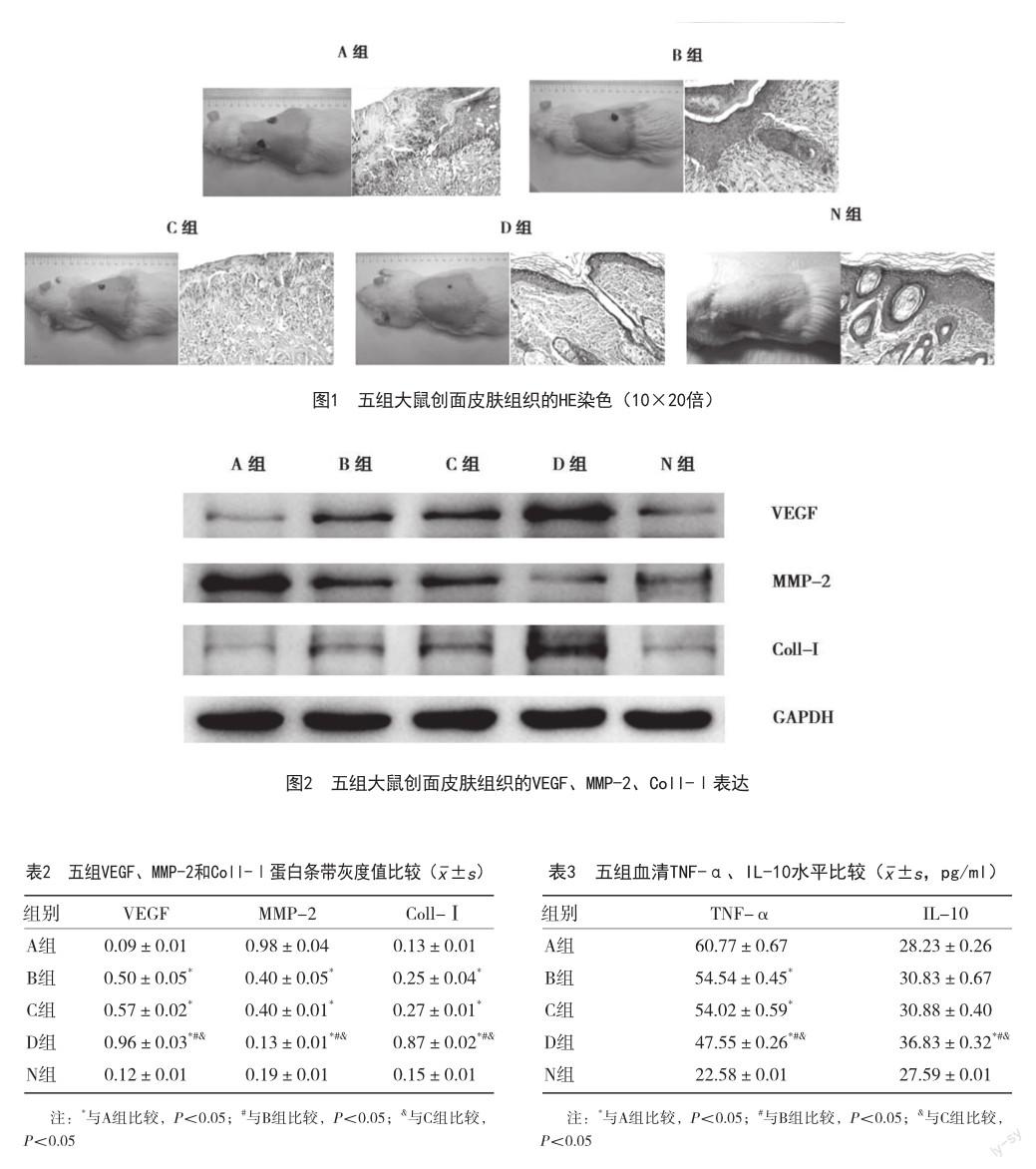
2.3 五组VEGF、MMP-2、Coll-Ⅰ蛋白表达水平比较 B组和C组VEGF、Coll-Ⅰ水平高于A组,MMP-2水平低于A组(P<0.05);B组和C组VEGF、Coll-Ⅰ、MMP-2水平比较,差异无统计学意义(P>0.05);D组VEGF、Coll-Ⅰ水平均高于A组、B组、C组,MMP-2水平均低于A组、B组、C组(P<0.05),见图2、表2。
2.4 五组血清TNF-α、IL-10水平比较 B组、C组TNF-α水平均低于A组(P<0.05);A组、B组、C组IL-10水平比较,差异无统计学意义(P>0.05);D组TNF-α水平均低于A组、B组、C组,IL-10水平均高于A组、B组、C组(P<0.05),见表3。
3 讨论
浅Ⅱ度烫伤常见于开水、热汤、热油造成的烫伤,以及持续时间比较短的火焰烧伤等,主要表现为真皮损伤,局部红肿疼痛,创面渗液较多,有大小不等的水疱,如不及时处理或处理不佳,会加重皮肤损伤程度,不仅减慢愈合时间,还可能会留下瘢痕,对患者的身体和心理产生一定的影响[5,6]。磺胺嘧啶银是治疗烫伤的一种常用的外用药物,其药效也在研究中得以证实[3],但容易造成皮肤局部刺激性、皮疹、皮炎、不良反应较多,甚至会导致创面组织脱水干燥,对烫伤后疼痛无缓解功效[7,8]。木犀草素是一种天然的黄酮类化合物,存在于桔梗、金银花等多种中药中,具有抗炎、抗氧化、抗过敏、抗肿瘤等多种药理活性,通过抑制氧化自由基成为抗皮肤衰老和炎症的调节剂[9-11]。研究发现[4],木犀草素是促进皮肤烫伤大鼠创面愈合的有效成分。也有实验发现[12],木犀草素对兔耳增生性瘢痕抑制作用,局部涂抹木犀草素可以改善小鼠干燥性皮肤瘙痒,均显示了木犀草素对于创面愈合的有益作用。为解决磺胺嘧啶银的诸多不良反应,本研究通过磺胺嘧啶银与木犀草素联合应用,通过检测创伤修复相关分泌因子以及炎症相关信号通路关键因子的表达情况,寻找潜在的机制。
本研究结果显示,D组第7天烫伤创面愈合率均高于A组、B组、C组(P<0.05);D组VEGF、Coll-Ⅰ、IL-10水平均高于A组、B组、C组,MMP-2、TNF-α水平均低于A组、B组、C组(P<0.05),提示磺胺嘧啶银和木犀草素联合治疗浅Ⅱ度烫伤的效果优于单独用药,可加快创面皮肤的结痂和愈合。分析磺胺嘧啶银联合木犀草素的作用机制可能是通过上调VEGF促进周围血管形成,下调MMP-2表达,上调Coll-Ⅰ表达,抑制透明质酸酶和胶原酶的活性,导致细胞外基质更加稳定,角质形成细胞从伤口边缘迁移,形成完整的细胞片[13],从而缓解由磺胺嘧啶银造成的创面组织脱水干燥、皮炎、皮疹等不良反应,增加角质形成细胞的伤口愈合能力;另一方面,通过上调IL-10表达,上调转录活化因子6(signal transduction and activator of transcription 6,STAT6)和抑制转录激活子3(signal transduction and activator of transcription 3,STAT3)[14],从而抑制单核巨噬细胞释放炎症介质,进一步抑制LPS和IFN-γ导致的TNF-α等因子分泌,实现对核因子κB(nuclear factor kappa B,NF-κB)、激活蛋白1(activator protein,AP-1)等转录因子的调控,从而调节NF-κB信号通路,提升抗炎活性,促进伤口愈合[15]。
综上所述,磺胺嘧啶银和木犀草素联合用药可促进浅Ⅱ度烫伤的创面皮肤愈合,提高临床有效率,可作为潜在的临床上治疗浅Ⅱ度烫伤的治疗方案之一。下一步,研究团队将对浅Ⅱ度临床烫伤患者进行磺胺嘧啶银和木犀草素联合用药的临床试验和进一步的机制探讨,以进行临床有效性和安全性的评估,为未来的研究提供更多的理论基础。
参考文献
[1] 孙萍,徐慧,黄艳红,等.桔梗化学成分的提取方法和药理作用概述[J].中国酿造,2022,41(9):18-23.
[2] 肖如雁,谢红莲,宋佳林,等.木犀草素对原发性硬化性胆管炎治疗作用研究[J].中国现代医生,2023,61(31):76-81.
[3] 宋萌,陈庆杰,王宏宇,等.外用rhGM-CSF凝胶联合磺胺嘧啶银乳膏治疗小面积深Ⅱ度难愈创面的疗效及安全性[J].解放军医药杂志,2019,31(5):67-70.
[4] Wang L,Hu L,Peng Z,et al.Luteolin is an Effective Component of Platycodon grandiflorus in Promoting Wound Healing in Rats with Cutaneous Scald Injury[J]. Clin Cosmet Investig Dermatol,2022,15:1715-1727.
[5] Shahzad MN,Ahmed N.Effectiveness of Aloe Vera gel compared with 1% silver sulphadiazine cream as burn wound dressing in second degree burns[J].J Pak Med Assoc,2013,63(2):225-230.
[6] 任雨洁,罗锦花,詹剑华.复方雪莲烧伤膏对深Ⅱ度烫伤创面愈合的作用及机制[J].南昌大学学报,2022,62(1):16-23.
[7] 简繁,赵守和,马森.磺胺嘧啶银软膏治疗烧伤创面的临床疗效观察[J].中国处方药,2022,20(2):82-83.
[8] 张宏峰,高栋梁,赵朋来.磺胺嘧啶银霜联合rhGM-CSF凝胶制剂治疗对深Ⅱ度烧伤创面溶痂的影响[J].海南医学,2022,33(7):887-890.
[9] Zhong L,Tang H,Xu Y,et al.Luteolin alleviated damage caused by blue light to Drosophila[J].Photochem Photobiol Sci,2022,21(12):2085-2094.
[10] Caporali S,De Stefano A,Calabrese C,et al.AntiInflammatory and Active Biological Properties of the PlantDerived Bioactive Compounds Luteolin and Luteolin 7-Glucoside[J].Nutrients,2022,14(6):1155.
[11] 张丽宏,张宁,刘国良,等.金银花有效成分木犀草素对UVB辐射致皮肤光老化保护作用研究[J].中医药学报,2016,44(3):27-30.
[12] 李泰平,肖红.木犀草素对兔耳增生性瘢痕抑制作用机制的初步研究[J].中国美容医学,2021,30(8):91-94.
[13] Gendrisch F,Esser PR,Schempp CM,et al.Luteolin as a modulator of skin aging and inflammation[J]. Biofactors,2021,47(2):170-180.
[14] Huang X,Dai S,Dai J,et al.Luteolin decreases invasiveness,deactivates STAT3 signaling,and reverses interleukin-6 induced epithelial-mesenchymal transition and matrix metalloproteinase secretion of pancreatic cancer cells[J].Onco Targets Ther,2015,8:2989-3001.
[15] Aziz N,Kim MY,Cho JY.Anti-inflammatory effects of luteolin:A review of in vitro,in vivo,and in silico studies[J]. J Ethnopharmacol,2018,225:342-358.
编辑 扶田



